Welcome to Swift Medical’s multi-part series: The Hospital Digital Wound Care Maturity Model.
What is the Digital Wound Care Maturity Model?
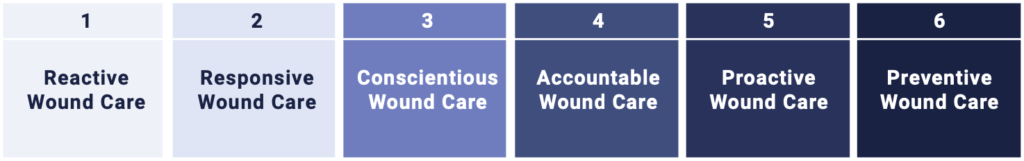
Wounds likely pose a far greater risk to your hospital than you realize. While they often don’t receive the same level of attention as cancer or heart failure, their impact can be even more profound.The Digital Wound Care Maturity Model is used to help understand the current-state of a hospital’s wound care program in order to guide the development of a more advanced, digitally-enabled approach going forward. The maturity model is a vendor-neutral framework designed to support the implementation and optimization of a hospital-centric wound care program. The model takes an evolutionary, staged approach to support adoption of increasingly advanced digital tools and technologies to elevate a clinical program and deliver superior clinical, operational, and economic outcomes.
In the previous entries in this series, we introduced the massive and poorly-understood wound care epidemic in hospitals, provided an overview of the model itself, discussed strategies for building a high-performing wound care team, explored how thoughtful governance structures can help drive best practice adoption, and detailed how adopting technology can enable improved clinical and economic performance for your organization.
In this installment, we will discuss how using data and analytics can drive improved care.
Part 6 – How Analytics Enable Data-driven Wound Care
Without the ability to capture, manage, and analyze data, organizations are severely limited in their capacity to make appropriate and timely clinical decisions.
The point-of-care imaging technologies mentioned in the previous entry in the series are critical to the collection of standardized, high-quality data. Analytics and AI are then vital to enabling clinicians and programs to act on the data to improve care.

At stages 1 and 2 of the maturity model (paper ruler measurement or rudimentary digital photography), the lack of a standardized, purpose-built tool for wound assessment and image capture inhibits almost all meaningful analysis and tracking of wound healing. Records may be incomplete and difficult to access without a centralized digital repository. Measurements may be recorded differently by different clinicians, presenting even further challenges when trying to obtain meaningful information from inaccurate and inconsistent wound data.
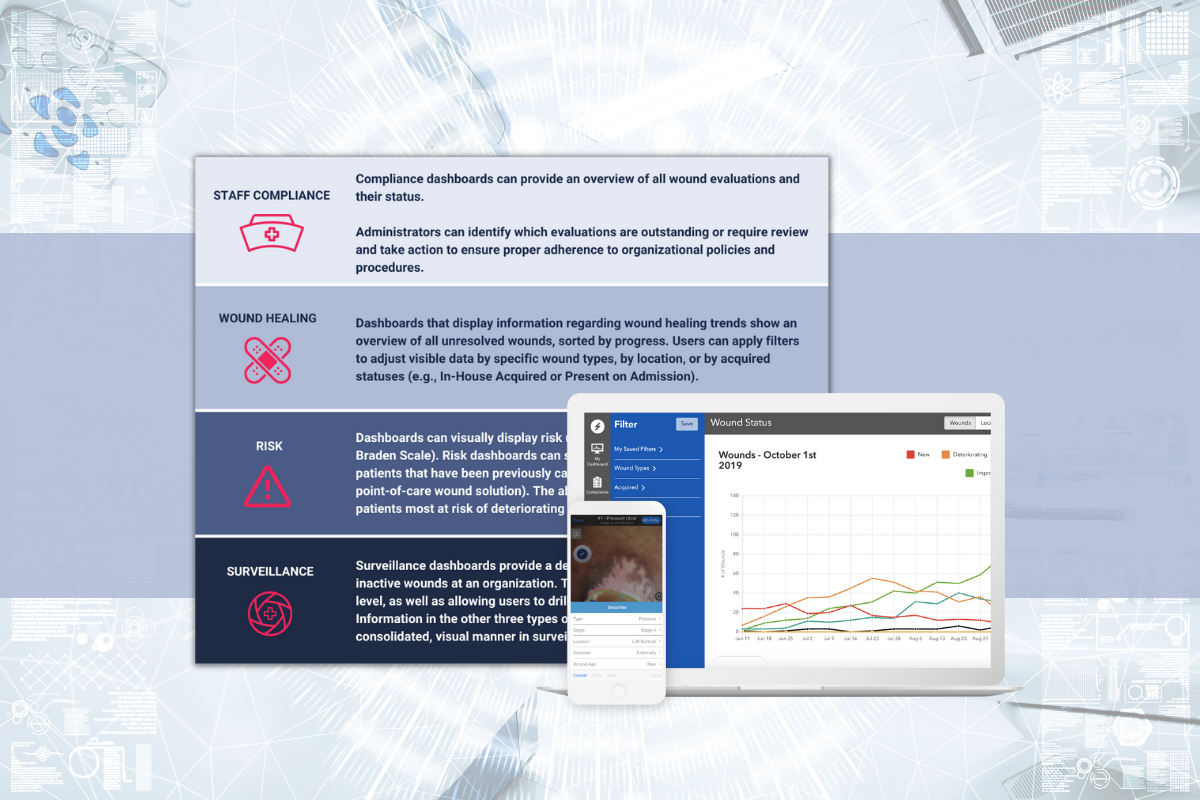
Organizations at Stages 3 and 4 (purpose-built digital wound measurement platforms) will begin to see the benefits of improved visibility into their wound program through data and improved reporting capabilities. One of the biggest benefits of dedicated digital wound applications is the ability to access and manage real-time data reports and dashboards. Organizations that rely on paper rulers to assess wounds may only access records retroactively, if at all. With access to real-time data, administrators can identify trends within their wound care program and make data-driven decisions to improve care delivery.
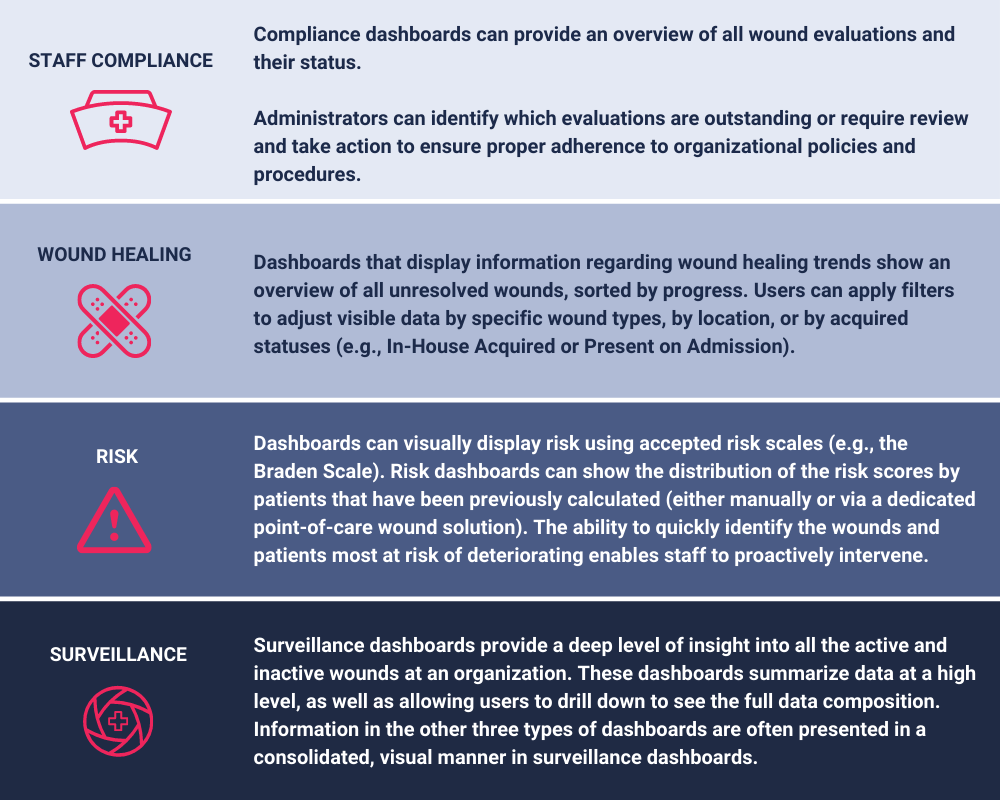
The table below details how dashboards can provide valuable insight into staff compliance, wound healing status, risk, and overall wound program surveillance.
In the next installment, we explore how an optimized, high maturity wound care program extends beyond the hospital walls and into the community and the home, connecting and coordinating care across the continuum.
Sign up for our mailing list to get notified directly of new blog posts.