Welcome to Swift Medical’s multi-part series: The Hospital Digital Wound Care Maturity Model.
What is the Digital Wound Care Maturity Model?
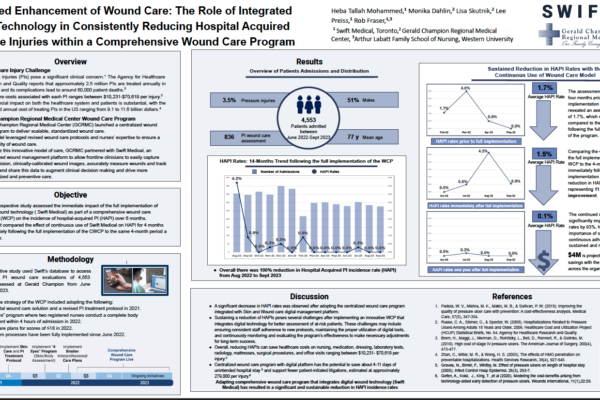
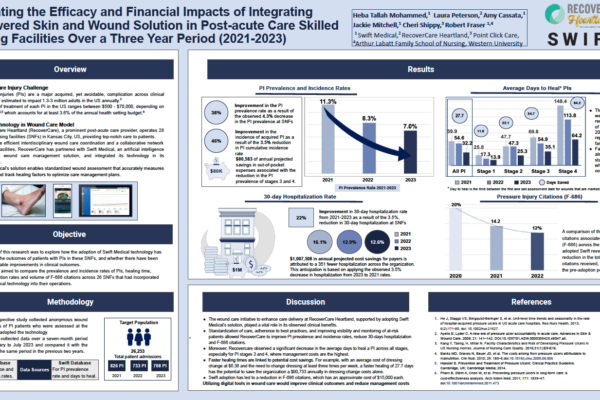
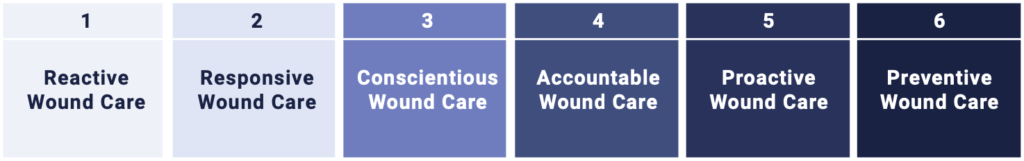
Wounds likely pose a far greater risk to your hospital than you realize. While they often don’t receive the same level of attention as cancer or heart failure, their impact can be even more profound.The Digital Wound Care Maturity Model is used to help understand the current-state of a hospital’s wound care program in order to guide the development of a more advanced, digitally-enabled approach going forward. The maturity model is a vendor-neutral framework designed to support the implementation and optimization of a hospital-centric wound care program. The model takes an evolutionary, staged approach to support adoption of increasingly advanced digital tools and technologies to elevate a clinical program and deliver superior clinical, operational, and economic outcomes.
In the previous entries in this series, we introduced the massive and poorly-understood wound care epidemic in hospitals, provided an overview of the model itself, discussed strategies for building a high-performing wound care team, and explored how thoughtful governance structures can help drive best practice adoption.
In this installment, we will discuss the transformative impact technology can play in improving operational efficiency, financial performance, and patient outcomes.
Part 5 – Technology’s Role in Improving Operational, Financial, and Clinical Outcomes
Technology is often hailed as a panacea in healthcare. However, introducing technology without a strong foundation of people, process, and policies (as described in the previous entries in this series) is bound to fail. That being said, the adoption of advanced digital technologies has been proven to significantly impact the quality of care an organization can deliver. Implemented thoughtfully, digital tools can reduce in-house acquired wounds, improve healing time, decrease assessment time, and reduce supply and staff costs, both in hospitals and across the continuum.

Manual Measurement Methods
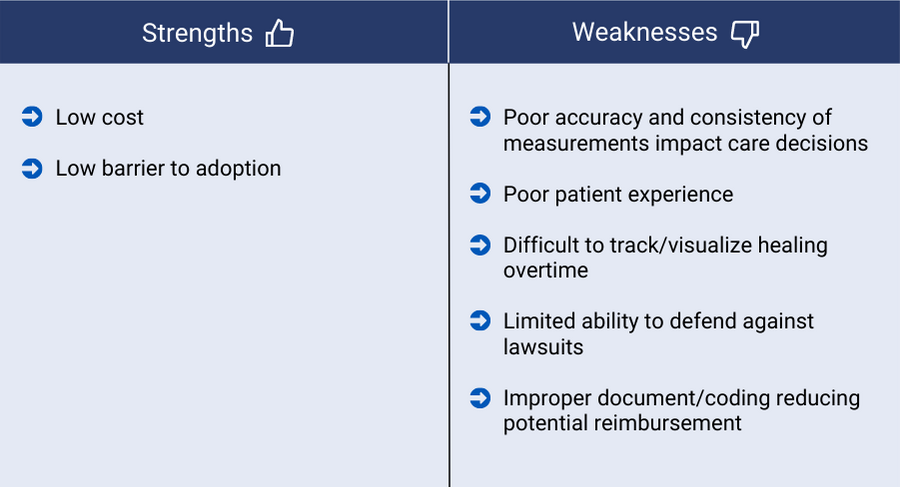
The adoption of new imaging technology in wound care is a key milestone in the overall progression of an organization through the Digital Wound Care Maturity Model. Many organizations begin their journey using paper rulers to measure wounds. The ruler method uses a disposable paper ruler to calculate the wound area, measuring the longest length by the widest width. A Q-tip is also often used to measure the deepest part of the wound.
While this method is low-cost and relatively easy to implement, its downsides are numerous. Studies have shown that the ruler method can lead to error rates upwards of 40%.¹ These errors can be further compounded when wounds are measured by different staff on different days.
Not only can inaccurate or missing documentation impact the quality of treatment decisions, a lack of proper wound documentation can create greater organizational risk. Sufficient wound documentation is often required to defend against pressure injury litigation (the second most common medical lawsuit). Further, proper documentation is also needed to ensure appropriate reimbursement from payers and reduce rejected claims.
Additionally, the use of a Q-tip to measure depth is often a painful and uncomfortable procedure for patients.
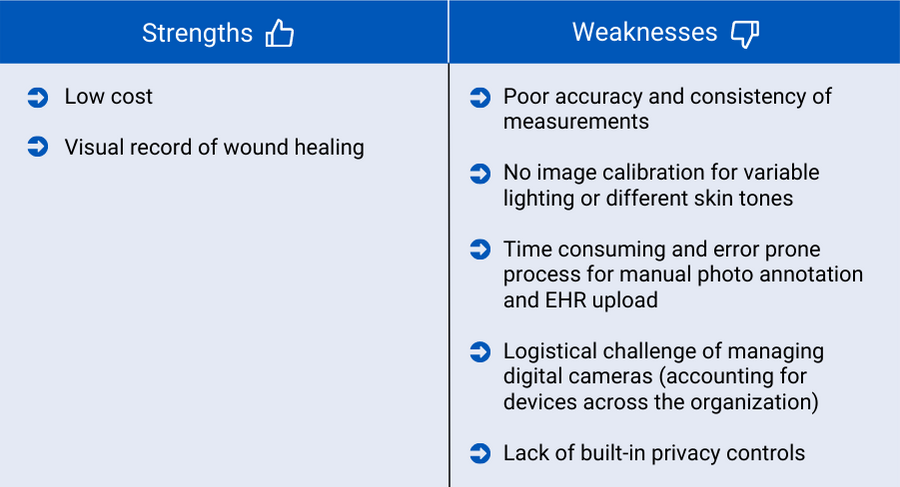
Digital Photography
As organizations advance their wound care programs, they often implement digital photography as the first aspect of technology in their wound program. Digital photography can be a useful tool for visually documenting wounds over time and digital cameras are low-cost and easy to use. However, digital photography alone still has many drawbacks. Images may be distorted due to lighting, body position, or distance from the camera to the wound. Cameras can go missing. And similar to using a paper ruler, clinicians may photograph the wound differently, making it more difficult to track healing. Without integration into an organization’s EHR, staff must spend time and risk making errors during the manual photo upload process. Perhaps the largest drawback to using consumer-grade digital photography is the lack of any built-in security or privacy controls for images after they have been captured.
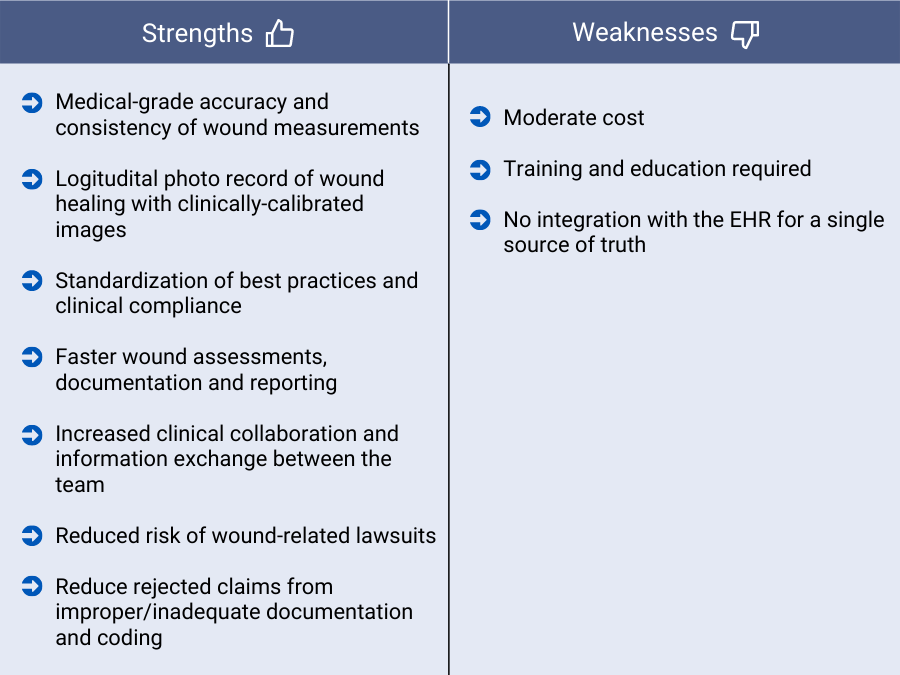
Point-of-Care Wound Imaging and Measurement Solutions
The implementation of a purpose-built, digital wound management solution is the first meaningful step into digital wound care. These solutions are often deployed as smartphone applications that leverage the device’s existing cameras. They have enforceable workflows, built-in security, and, in many cases, imaging technology that automatically adjusts for lighting, position, and color. Many of these solutions can automatically trace wounds and calculate surface area and depth without the need to physically touch the patient. Without dedicated wound measurement technology, assessments completed using a paper ruler or digital camera suffer from poor accuracy, precision, and reliability between different assessors.
The adoption of a purpose-built digital wound imaging and assessment tool, even if not widely implemented, opens the door for the early stages of data driven wound care. Tools that are designed to digitally record wound measurements include the capacity to centrally store and manage information in one place, unlocking crucial information about the healing trajectory of wounds. The adoption of a dedicated digital wound application not only improves the technical capacity of a wound team, it also provides a means to disseminate standardized wound care best practices.
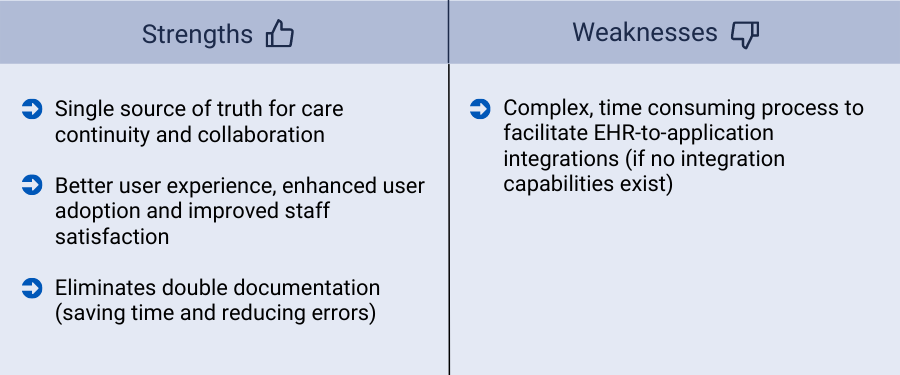
EHR Integration
As with the implementation of any specialized digital health solutions, integration with the hospital EHR is imperative. This is especially true with wound care technology, as the interdisciplinary nature and long healing time of wounds require interaction with many clinicians, often expanding to multiple hospital departments and care settings. Ensuring that the entire care team has seamless access to accurate patient and wound information from the EHR allows for better quality and continuity of care for complex wounds.
By fully integrating their digital wound solution with their EHR, clinicians get more information about a patient’s overall health when treating wounds and more insight into wound healing when treating a patient for other reasons. Organizations also realize more time-saving and efficiencies through reduced duplicate documentation and streamlined workflows.
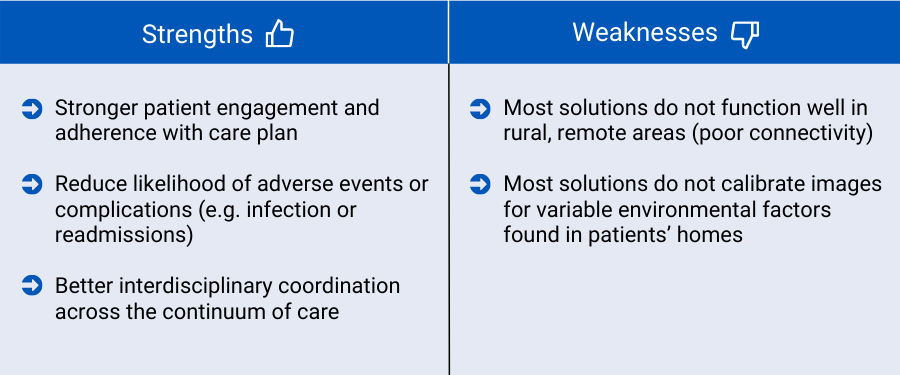
Remote Patient Monitoring
The implementation of remote patient monitoring technology allows for care management and visibility to extend beyond the hospital walls, while engaging the patient as a key member of their own wound management. A patient application can help providers continue to monitor wound healing and patient risk, as patients or caregivers can use their mobile phone to capture photographs of their wounds and securely share them with the care team. It can be used in combination with in-person visits without having to go into a clinic.
The use of telemedicine and telewound care provides more convenience and comfort for patients who prefer to receive care at home or who may live in rural settings. Studies have shown that involving wound care patients in their own care improves patient engagement and leads to improved clinical outcomes through increased access to education and adherence to treatment guidelines.²
Physiological Imaging
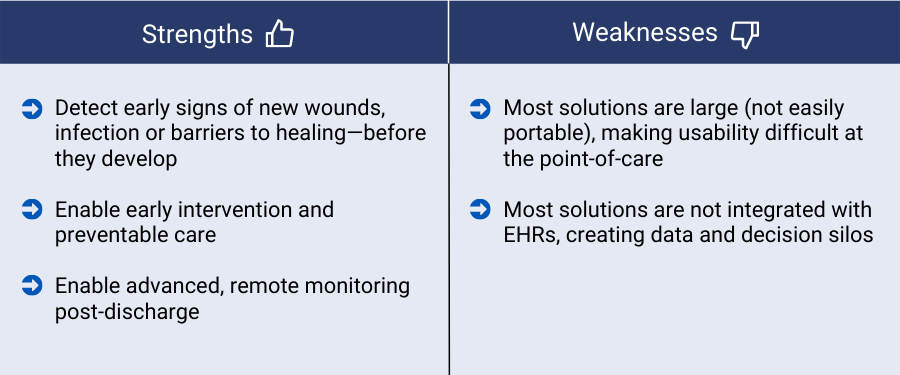
The latest frontier in digital wound management has seen the adoption of technologies that transcend imaging in the visible spectrum with new technologies that enable clinicians to look beneath the surface skin. Thermal imaging in the longwave infrared spectrum (LWIR), violent fluorescent imaging, and imaging in the near-infrared spectrum all have tremendous potential to transform wound care. These noninvasive techniques promote proactive intervention by allowing clinicians to see patterns of heat, blood flow, bacterial colonization, and blood oxygenation. These patterns can be used to identify the earliest signs of new wounds before they become visible to the naked eye on the surface of the skin.
These technologies have tremendous potential to improve care. Some examples include:

Using new physiological imaging technology opens the door to new data-driven insights, as clinicians and researchers gain access to a host of new data points on temperature, blood flow, and bacterial growth. This new trove of information can be used to train the next generation of predictive wound healing algorithms.
The progression of steadily more advanced technologies is a key component of the Digital Wound Care Maturity Model and a crucial factor in improving the overall performance of your wound care program. And while the right team and governance is an important prerequisite for a high-performing organization, it is advances in technology that will ultimately help wound care advance as a discipline in the same way that other specialties have in recent years.
In the next installment, we will explore how the data produced by digital wound tools enables improved visibility and risk monitoring via advanced analytics.
Sign up for our mailing list to get notified directly of new blog posts.
¹ Schultz G, Mozingo D, Romanelli M, Claxton K. Wound healing and TIME; new concepts and scientific applications. Wound Repair Regen. 2005 Jul-Aug;13(4 Suppl):S1-11. doi: 10.1111/j.1067-1927.2005.1304S1.x. PMID: 16008735.
² Wang SC, Anderson JA, Jones DV, Evans R. Patient perception of wound photography. Int Wound J. 2016 Jun;13(3):326-30. doi: 10.1111/iwj.12293. Epub 2014 May 28. PMID: 24872018; PMCID: PMC79501