Welcome to Swift Medical’s multi-part series: The Hospital Digital Wound Care Maturity Model.
What is the Digital Wound Care Maturity Model?
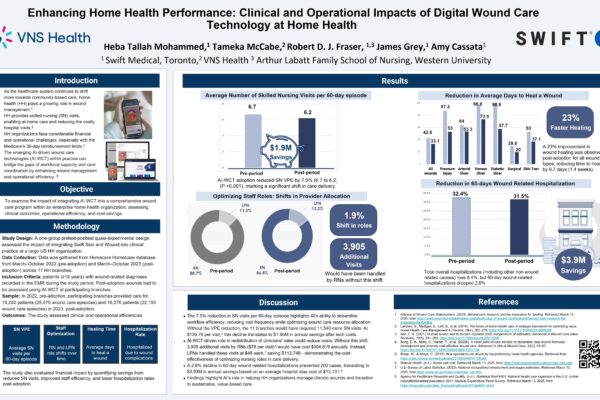
Wounds likely pose a far greater risk to your hospital than you realize. While they often don’t receive the same level of attention as cancer or heart failure, their impact can be even more profound.The Digital Wound Care Maturity Model is used to help understand the current-state of a hospital’s wound care program in order to guide the development of a more advanced, digitally-enabled approach going forward. The maturity model is a vendor-neutral framework designed to support the implementation and optimization of a hospital-centric wound care program. The model takes an evolutionary, staged approach to support adoption of increasingly advanced digital tools and technologies to elevate a clinical program and deliver superior clinical, operational, and economic outcomes.
In the previous entries in this series, we introduced the massive and poorly-understood wound care epidemic in hospitals, provided an overview of the model itself, and discussed strategies for building a high-performing wound care team.
In this installment, we will discuss some governance strategies designed to help optimize the performance of a hospital’s wound program.
Part 4 – Improving Wound Program Governance to Drive Best Practice Adoption
Governance is critical to implementing and optimizing quality improvement programs. This is especially true for complex, hierarchical and multi-departmental organizations, such as hospitals.
A high performing wound care program depends on overall governance structure and several key processes driven by dedicated working groups, as detailed in the diagram below.

| Key Processes / Working Groups | Core Responsibilities | Example Membership | Operational Frequency |
|---|---|---|---|
| Steering Committee | – Overall development and ongoing performance management of wound care program and fulfillment of KPIs – Review monthly/quarterly reports and make recommendations on operation and evolution of the program – Review and make final decisions on recommendations from each of the sub-groups |
– CNO – Wound Care Lead – Quality Assurance – Risk Management – CMO |
Quarterly |
| Best Practice Guidelines (BPG) Reviews, Updates and Education | – Develop/implement standardized clinical best practice guidelines (e.g. treatment of DFUs, prevention of pressure injuries) – Develop/implement best practice organizational policies (e.g. consult process, risk screening) – Regular review and updating of guidelines/policies based on medical literature – Lead wound care training and education across all clinical units |
– DON – Education Wound Care Lead – Wound Care – Physician Lead Informatics |
Bi-annually |
| Product/Supply Inventory Management | – Implement standardized formulary management plan – Monitor product/supply utilization and inventory to drive forecasting and fulfillment – Evaluate new products and technologies for potential adoption |
– Wound Care Lead – Wound Care Physician Lead – Supplies Management – Informatics – The Vendor(s) of Record |
Monthly |
| Wound Council / Patient Chart Reviews | – This multidisciplinary team meets to review complex/stalled wounds and determine correct course of action – Common scenarios/lessons learned are indexed and shared with BPG team |
– Wound Care Lead – Risk Management Utilization – Informatics – Legal |
Weekly |
| Wound Incident/Event Reviews | – Root cause analysis of adverse or sentinel events – Development of recommendation to BPG team to develop new policies/protocols to mitigate adverse events |
– Wound Care Lead – DON – Risk Management – Informatics – Legal – Ethics |
Monthly |
Incorporating Guidelines and Best Practices
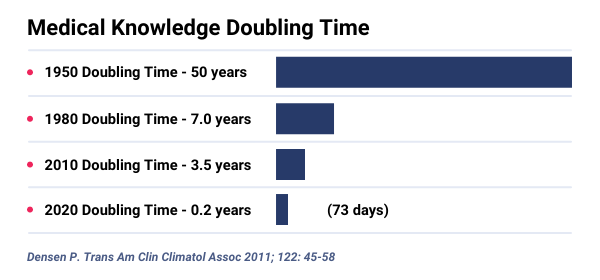
Once an established governance structure is in place, it can play an important role in ensuring that the latest best practices make their way to the point of care as part of an organization’s wound care program. Healthcare information is expanding too fast for clinicians to remain current with all relevant recommendations for best practice. The volume and sources of information growth has exceeded human capacity and traditional methods for keeping up to date are no longer sustainable. Providing standardized, evidence-based care is more challenging than ever.
Establishing standardized, evidence-based wound management best practices is critical to ensuring every patient receives the highest quality of care while appropriately utilizing resources. By aligning your clinical practices with best practices, you’ll be able to ensure all your staff provide the most efficient and effective care.
A few key areas of clinical standardization include:
- Formulary – Create a standardized wound formulary to drive supply chain optimization and ensure appropriate product formulary is used for each patient. This will optimize wound healing, patient outcomes and resource utilization, ultimately driving down supply costs and increasing your margin.
- Best Practice Guidelines and Care Pathways – Develop organizational best practices and policies that guide frontline staff regarding wound assessment, documentation, and ongoing management. Wound care protocols and pathways will standardize clinical decision making across your organization, ensuring everyone is confident and consistent in their clinical decision-making and operating at the top of their license.
- Patient Education – Provide patients with evidence-based educational resources about how to properly manage their wounds and recognize signs of improvement or deterioration—especially in preparation for hospital discharge. By making patients active participants in their care journey, you empower them with knowledge and allow them to take greater responsibility for their health and healing.
Borrow from the Best!
Rather than beginning from scratch, you can leverage the work of trusted clinical expert groups and wound care associations to adopt and adapt Best Practice Guidelines. The following organizations have created wound care guidelines, protocols and tools that can be used to develop or adapt wound care policies and protocols for your organization.
- Wound Healing Society
- Wound, Ostomy and Continence Nurses Society
- National Pressure Ulcer Advisory Panel
- Cochrane Database
- Wound Care Education Institute
- Peer-reviewed paper in reputable medical journals (e.g.. Journal of Wound Care,JAMDA)

Further, healthcare quality organizations such as the Agency for Healthcare Research and Quality (AHRQ) have developed in-depth toolkits and modules to help organizations to implement best practices. One such resource is the AHRQ’s Preventing Pressure Ulcers in Hospitals, which includes modules such as Best Practices in Pressure Injury Prevention, which provides training guides, presentations, checklists and tools to support the practical implementation of a pressure injury program.

What’s Next: Standardization at its Finest
Developing and implementing best practice guidelines is a great start, but will ultimately fail to standardize evidence-based care in the long run if they are not: a) accessible to clinicians at the point-of-care, b) kept current to reflect the most current evidence, and c) augmenting complex clinical decision making at the bedside.
| Accessible at the Point-of-Care | If Best Practice Guidelines aren’t easily accessible at the point-of-care, they have no value. Guidelines need to be integrated with and accessible through digital tools used for wound care at the bedside (e.g., EHR or wound imaging application). Similarly, if patient education materials and resources can be shared with the patient in a convenient, digital manner (e.g., hospital portal or patient monitoring application), they are more likely to adhere to care plans. |
|---|---|
| Up-to-Date with Latest Evidence & Hospital Policy |
If guidelines aren’t reviewed and updated regularly, they will no longer reflect the most recent medical evidence and clinical practices. A dedicated working group can be established within the wound care governance structure to complete annual guideline reviews and make required revisions. With sophisticated wound management solutions, analytics can demonstrate the correlation between treatments and outcomes for patient cohorts to further refine guidelines based on real-world evidence. |
| Dynamic & Personalized Decisions Support | Most commonly, best practice guidelines and pathways are static documents, based on genetic diseases/conditions and population-based evidence. However, with large wound datasets that capture both clinical inputs and outputs (treatments and outcomes), more dynamic, precise, and personalized treatments can be recommended to clinicians based on their patients unique demographic and clinical characteristics. |
With the right team, governance structure, and best practice guidelines in place, a hospital is well poised to adopt new technologies. Our next entry discusses the impact of new technologies and how to maximize their transformative potential for your organization.
Sign up for our mailing list below to get notified directly of new blog posts.