Welcome to Swift Medical’s multi-part series: The Hospital Digital Wound Care Maturity Model.
What is the Digital Wound Care Maturity Model?
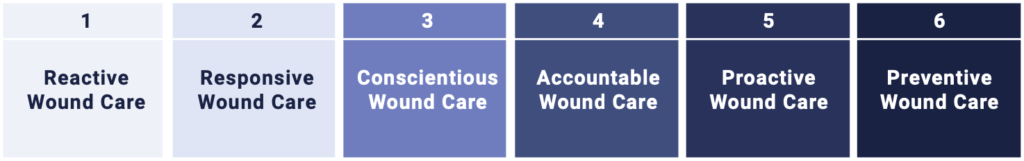
Wounds likely pose a far greater risk to your hospital than you realize. While they often don’t receive the same level of attention as cancer or heart failure, their impact can be even more profound.The Digital Wound Care Maturity Model is used to help understand the current-state of a hospital’s wound care program in order to guide the development of a more advanced, digitally-enabled approach going forward. The maturity model is a vendor-neutral framework designed to support the implementation and optimization of a hospital-centric wound care program. The model takes an evolutionary, staged approach to support adoption of increasingly advanced digital tools and technologies to elevate a clinical program and deliver superior clinical, operational, and economic outcomes.
Over the next several weeks, this series will cover:
- The main wound care challenges faced by hospitals
- The benefits of investing in wound care
- The evolutionary stages of the wound care maturity model
- A framework to help you understand the current state of your program
- Multiple strategies to advance your wound care program and clinical/economic outcomes
Part 1 – The Hospital Wound Care Epidemic
Wounds – The Silent Epidemic
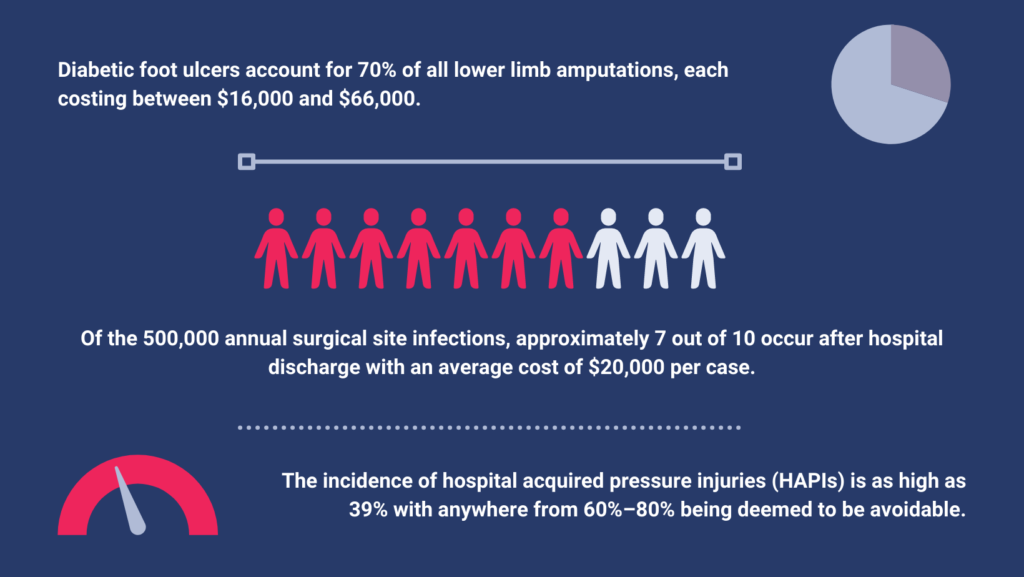
Wounds are often considered the silent epidemic in healthcare. Patients with wounds frequently suffer from other, more eminent conditions such as diabetes or hypertension, which obscure the severe impact of wounds. Nationally, there are over 8.2 million patients with wounds, which costs Medicare up to $96 billion annually. The annual direct costs associated with chronic wounds—in particular diabetic foot ulcers—are greater than the five most costly cancers in the US (breast, colorectal, lung, prostate, and leukaemia).
In hospitals, 15-40% of beds are occupied by a patient with a wound. The most prevalent types of wounds are diabetic foot ulcers, surgical wounds, and pressure injuries—each presenting massive clinical and financial challenges for hospitals and health systems.
The Hospital Wound Care Challenge
Wounds are highly prevalent, highly complex, and highly costly conditions that can greatly impact the clinical, operational, and financial performance of a hospital.

Our next installment of our Digital Wound Care Maturity Model Series discusses the different stages of the maturity model in more detail to help you understand the current state of your hospital wound care program – and how to take the next step in advancing the quality and digital maturity of your organization.
Sign up for our mailing list to get notified directly of new blog posts.
[1] Chandan K. Sen. Human Wounds and Its Burden: An Updated Compendium of Estimates. Advances in Wound Care. 2019.
[2] Neal R. Barshes, et al. The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabetic Foot and Ankle. 2013.
[3] Courtney H. Lyder, Elizabeth A. Ayello. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. 2008.
[4] Berríos-Torres SI, Umscheid CA, Bratzler DW, et al.. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017. JAMA Surg. 2017;152(8):784.
[5] Sanger PC, Simianu VV, Cameron GE, et al. Diagnosing Surgical Site Infection using Wound Photography: A Scenario-Based Study. J Am Coll Surg. 2017 January ; 224(1): 8–15.
[6] Shepard J, Ward, et al. Financial impact of surgical site infections on hospitals: the hospital management perspective. JAMA Surgery. 2013.
[7] Chandan K. Sen. Human Wounds and Its Burden: An Updated Compendium of Estimates. Advances in Wound Care. 2019.
[8] Caroline E. Fife, et al., Wound Care Outcomes and Associated Cost Among Patients Treated in US Outpatient Wound Centers: Data From the US Wound Registry, WOUNDS. 2012.
[9] Alok Raghav, et al. Financial burden of diabetic foot ulcers to the world: a progressive topic to discuss always. Therapeutic Advances in Endocrinology and Metabolism. 2018.
[10] Andreas F. Mavrogenis, at al. Current concepts for the evaluation and management of diabetic foot ulcers. EFORT. 2018. + Morteza Mahmoudi, Lisa J Gould.Opportunities and Challenges of the Management of Chronic Wounds. Chronic Wound Care Management and Research. 2020
[11] Courtney H. Lyder, Elizabeth A. Ayello. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. 2008.
[12] Joyce Pittman, et al. Hospital-Acquired Pressure Injuries in Critical and Progressive Care: Avoidable Versus Unavoidable. American Journal of Critical Care. 2019. + I Bales. Reaching for the moon: achieving zero pressure ulcer prevalence, an update. Journal of Wounds Care. 2009.
[13] Sunniva Zaratkiewicz, et al. Development and Implementation of a Hospital-Acquired Pressure Ulcer Incidence Tracking System and Algorithm. Journal for Healthcare Quality. 2010.
[14] Angela Christine Chang, et al.. A Comparison of Wound Area Measurement Techniques: Visitrak Versus Photography. ePlasty Web. 2014, 2011. + Louis D. Photographing pressure ulcers to enhance documentation. Decubitus. 1992.
[15] Yunghan Au and Sheila C Wang. Financial and Clinical Risk Evaluation of Pressure Injuries in US Hospitals: A Business Case for Initiating Quality Improvement. WOUNDS. 2019.
[16] Lanau-Roig, Anna, et al. Time of chronic wound healing, as part of a prevalence and incidence study. Enfermería Global. 2017.
[17] Chandan K. Sen. Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Advances in Wound Care. 2021
[18] Morteza Mahmoudi, Lisa J Gould.Opportunities and Challenges of the Management of Chronic Wounds. Chronic Wound Care Management and Research. 2020
[19] Cynthia A. Walker, et al. Hospitalists’ Needs Assessment and Perceived Barriers in Wound Care Management: A Quality Improvement Project. Journal of Wound Ostomy Continence Nursing. 2019.
[20] Anna T. Mayo and Anita Williams Woolley. Teamwork in Health Care: Maximizing Collective Intelligence via Inclusive Collaboration and Open Communication. AMA Journal of Ethics. 2016.
[21] Courtney H. Lyder, Elizabeth A. Ayello. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. 2008.
[22] Shah MK, Gandrakota N, Cimiotti JP, Ghose N, Moore M, Ali MK. Prevalence of and Factors Associated With Nurse Burnout in the US. JAMA Network Open. 2021.
[23] See citations 5,8 and 12.
[24] Courtney H. Lyder, Elizabeth A. Ayello. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality. 2008.
[25] Harold Brem, et al. High Cost of Stage IV Pressure Ulcers. American Journal of Surgery. 2010.
[26] Wound Care Education Institute. Legal Risks for Clinicians. https://promotions.wcei.net/wound-care-matters-resources