Welcome to Swift Medical’s multi-part series: The Hospital Digital Wound Care Maturity Model.
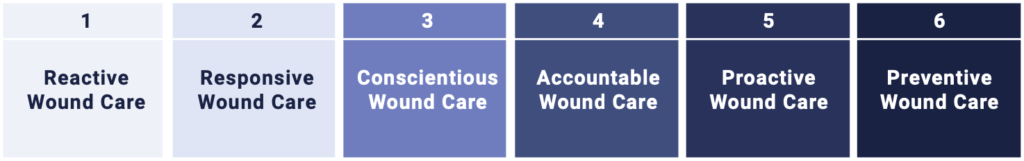
What is the Digital Wound Care Maturity Model?
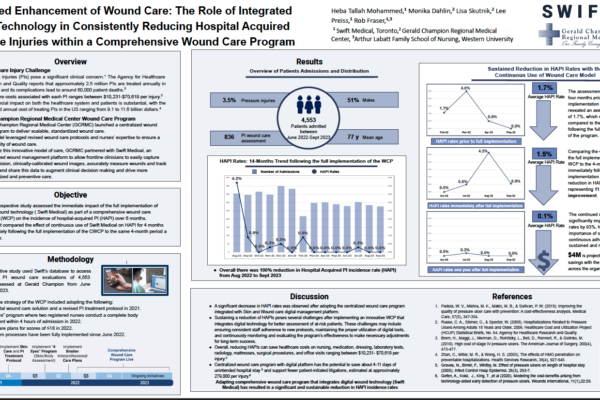
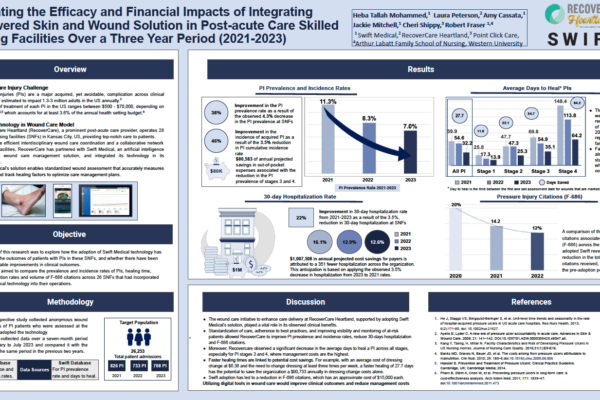
Wounds likely pose a far greater risk to your hospital than you realize. While they often don’t receive the same level of attention as cancer or heart failure, their impact can be even more profound.The Digital Wound Care Maturity Model is used to help understand the current-state of a hospital’s wound care program in order to guide the development of a more advanced, digitally-enabled approach going forward. The maturity model is a vendor-neutral framework designed to support the implementation and optimization of a hospital-centric wound care program. The model takes an evolutionary, staged approach to support adoption of increasingly advanced digital tools and technologies to elevate a clinical program and deliver superior clinical, operational, and economic outcomes.
In the previous entries in this series, we introduced the massive and poorly-understood wound care epidemic in hospitals, provided an overview of the model itself, discussed strategies for building a high-performing wound care team, explored how thoughtful governance structures can help drive best practice adoption, detailed how adopting technology can enable improved clinical and economic performance for your organization and examined the important role of analytics in managing risk and improving care.
In this installment, we will discuss how high-performing wound programs need to think beyond the walls of the hospital in order to provide the best possible care for patients.
Part 7 – The Importance of Wound Care Beyond the Walls of the Hospital
Chronic wounds can afflict patients for months, years, and even decades. Due to their persistent presence, wound patients typically require serial visits with multiple providers across different parts of the healthcare system before and after a hospital stay. Often there is minimal integration between settings and limited communication between providers. This leads to:
- An incoherent picture of the patient’s health history
- Poor care collaboration
- Inefficiencies due to duplicative or unnecessary treatments
- Adverse events and complications, such as infection, hospitalization or amputation
An optimized, high maturity wound care program extends beyond the hospital walls and into the community and the home, connecting and coordinating care across the continuum. Building referral relationships with other providers in your community is critical to an approach which supports your patients across their entire care journey. It ensures your clinicians stay abreast of patients’ wound healing progress and prevent deterioration or adverse events before they even happen.

The Connective Tissue: Technology Infrastructure for Integrated Care Delivery
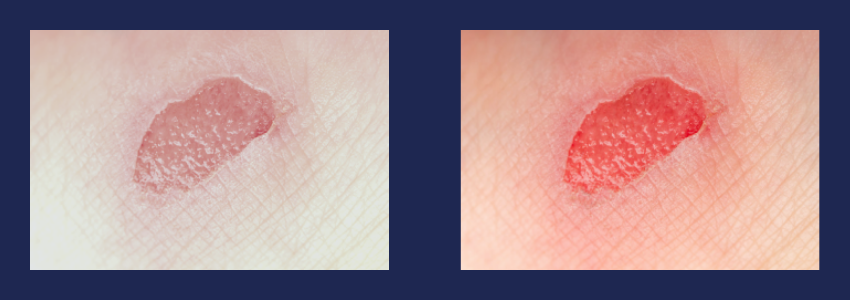
Wound care is a visually demanding medical discipline. As such, traditional modes of medical communication (telephone, EMR notes, photographs and even video-based telemedicine) fail to foster high quality clinical collaboration and coordination in wound care. To appropriately assess wound healing and provide clinical input remotely, high resolution, scientifically calibrated images are required, with sub-millimeter accuracy and lighting and color calibration to adjust for various environmental factors.
According to the American College of Tissue and Wound Repair, doctors often rely on visual assessments to determine the level of care needed for a chronic wound, and aspects of the healing process could be easily missed over the phone or a poor-quality video call. Other senses like touch, smell and temperature are also important when assessing wound healing and risk—all elements that are lost in remote care using common medical communication methods and solutions.
Hospital and health systems that wish to implement a high maturity, cross-continuum wound care program must think about adopting a wound management platform that can be used by clinicians, patients and caregivers in any clinical or domestic setting to enable consistent and collaborative wound care across the patient’s entire wound care journey.
In the next and final installment of the series we will be offering a self-assessment that will help you place yourself on the model to determine what strategies you can implement to improve the performance of your wound program.
To get notified directly when part 8 of our Digital Wound Care Maturity Model series is released, sign up for our mailing list below.