Good clinical practice starts with good clinical documentation. How can you know how well you are doing for your patients if you don’t document what you are doing and the results of your care.
During a recent webinar entitled “Legal Perils and Pitfalls of Wound Care” Heidi Cross provided some useful tips on documentation. Here are the top ten tips regarding good documentation practice and some do’s and don’ts.
1. VISUAL INSPECTION

Start by looking and describing what you see. It’s important to make consistent, accurate notes on both the patient and their skin (and or wound).
2. PRESSURE INJURY RISK ASSESSMENT


When specifically looking at the risk of pressure injury, ensure a full skin and patient assessment. Know which scoring system is used and ensure the correct score is recorded for your patient.
3. PRECISE USE OF LANGUAGE
Clear communication is important. A critical component of good communication is language. Language is important on so many fronts both with respect to your continued understanding and assessment of the patient with time; to communicating with others in the care team and sadly, if required, in a court of law to justify your actions.
4. PERTINENT INFORMATION TO INCLUDE


Ensure the pertinent information is recorded in your documentation. This is important for understanding or care given and resultant outcome. As is often stated “a picture paints a thousand words” so photography is a key component of pertinent information. But it not the only record and information required. Be as complete and descriptive as you can.
5. WOUND CATEGORY CHANGES
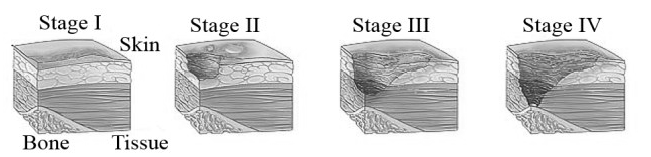
Pressure injuries should be recorded and staged. It’s a requirement of clinical practice. Staging and re-staging with time is vital to demonstrate changes in wound status. Also be careful not to miscategorise other wounds as pressure injuries as it has real, significant consequences. Especially with reporting.
6. PATIENT BEHAVIORS
If any patient behaviour has an impact on your ability to deliver care it is important that you document what and why? Try not to judge but rather document the facts as they occur. We all know what its like to be a patient so have some empathy to why their behaviour is what it is.
7. REFUSAL OF TREATMENT


As with each and everyone of us we have the absolute right to refuse any aspect of our care. Patients therefore have that right. It is important to record this and to record it accurately and how you think it will impact their care. More importantly record any education or corrective actions you may have taken to influence the patients decision.
8. HIPAA-APPROPRIATE PHOTOGRAPHY


Quality, safety and privacy is vitally important when handling patient information. This is especially true when handling photographs. There are rules and regulations provided by HIPAA to protect patients and it is important that such regulations are adhered to in each and every case.
9. END-OF-LIFE WOUNDS


End of life is a special circumstance and requires significant empathy. It is important to identify such wounds and to ensure appropriate care is provided. Of more importance is the documentation of the end-of-life status. These are special circumstances and skin failure is inevitable and a consequence of the process.
10. UNAVOIDABLE PRESSURE INJURIES


Unavoidable pressure injuries are a fact of life. More importantly they need to be recognized and documented. CMS recognizes unavoidable pressure injuries but requires early recognition and also the assurance that best practices were implemented to provide optimal care, both early in the diagnosis but more importantly ongoing.







