About once a week a small group of employees from Swift Medical Inc., visits a wound clinic to see first-hand the chronic wounds that make life so difficult for millions of people around the world.
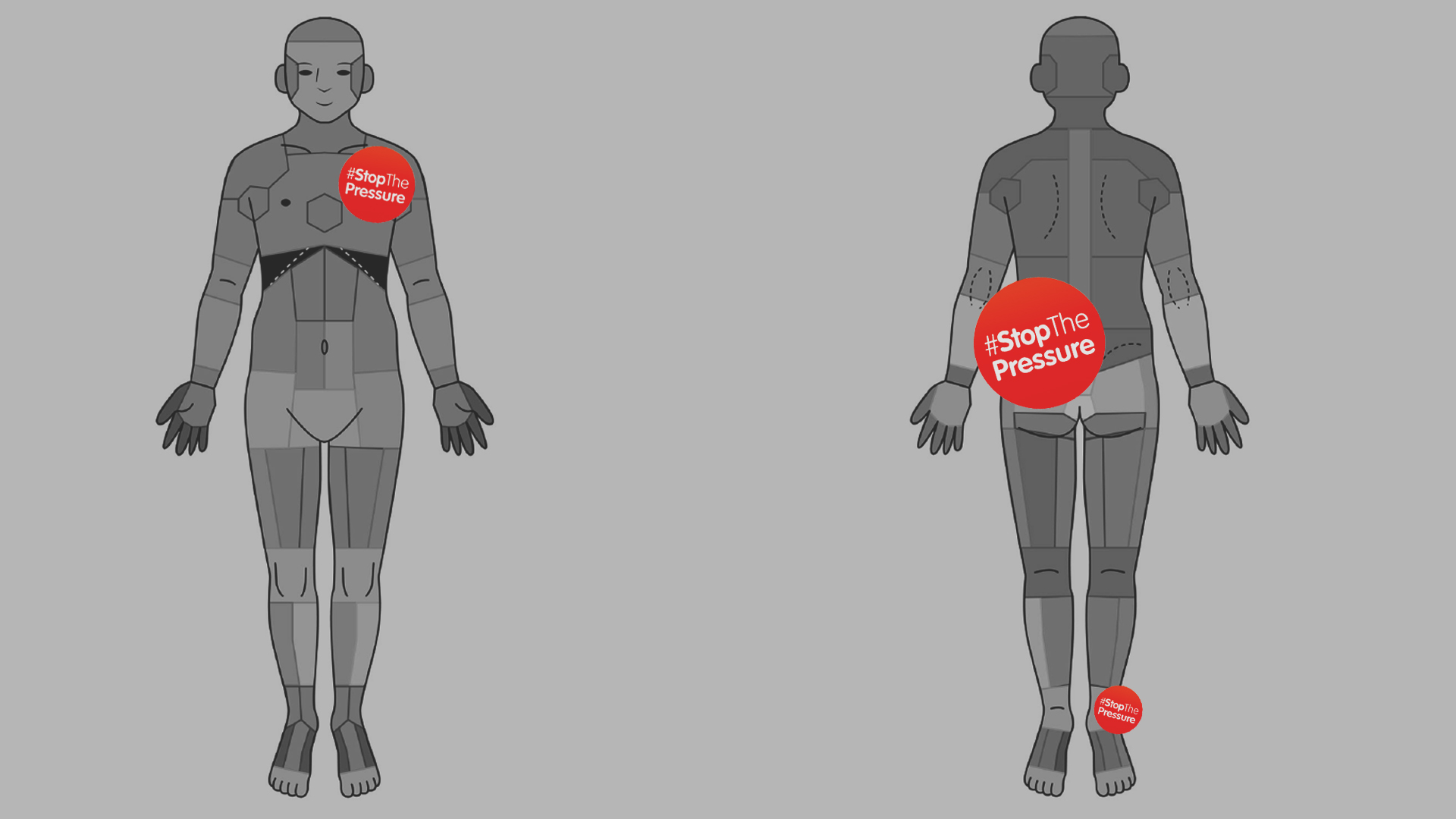
Many of the patients we see are diabetics and elderly people with mobility challenges. Their wounds typically fall into the category of pressure ulcers — lesions caused by pressure or friction against the skin. A recent Swift analysis of common wound locations among nursing home residents found pressure ulcers are most frequently located in the tailbone area, heels, buttocks and the bottom part of the pelvis where most of our weight rests when we sit.
Also known as bedsores, pressure ulcers are a serious and potentially fatal medical condition that affects 2.5 million people in the United States each year. In U.S. healthcare facilities, almost one in 10 patients and residents struggle with pressure ulcers.
Globally, more than 305 million serious and chronic wounds are recorded and treated each year — more than nine times the total number of people around the world living with cancer.
Our wound clinic visits are mandatory for all Swift employees, some of whom already work daily with care providers across the entire spectrum of healthcare settings. These visits can be hard to take, especially for new team members who have never seen a chronic wound up-close. But they are valuable reminders that the challenges we’re addressing here at Swift are, ultimately, not about writing the next line of code and improving algorithms but rather real human suffering on a massive scale.
That’s why today is an especially important day for us at Swift. Around the world, organizations and individuals are calling for efforts to “Stop the Pressure” for International Stop Pressure Ulcer Day. The movement is punctuated eloquently by a red dot — a symbol that evokes the concentration of pain from just one pressure ulcer, not to mention the hours and resources it takes to treat and care for a chronic wound.
The good news is we’re making progress. Between 2006 and 2015, the overall prevalence of pressure ulcers in all healthcare facilities in the U.S. declined from 13.5% to 9.3% — the result of greater awareness and more stringent regulations around making pressure ulcers a “never event.” Advances in methods to measure, treat and manage wounds have also made a big difference.
But we can — and must — do better. Pressure ulcers typically affect those who are already vulnerable: people who are sick or elderly. Here are Swift, we continue to push for better clinical and administrative workflows around wound care management. Today, we’ve all pinned on a #Stop the Pressure red dot to get more people talking about pressure ulcers and other types of chronic wounds.
We invite you to join us in our mission by spreading the word about Stop the Pressure. Forward this blog or mention it on Facebook or LinkedIn. Tweet about it using hashtag #StopthePressure. Let’s start and keep the conversation going about pressure ulcers and chronic wounds.