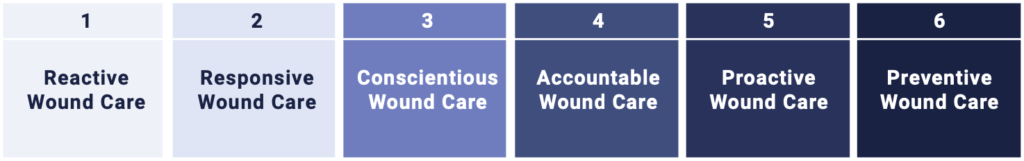
Welcome to Swift Medical’s multi-part series: The Hospital Digital Wound Care Maturity Model.
What is the Digital Wound Care Maturity Model?
Wounds likely pose a far greater risk to your hospital than you realize. While they often don’t receive the same level of attention as cancer or heart failure, their impact can be even more profound.The Digital Wound Care Maturity Model is used to help understand the current-state of a hospital’s wound care program in order to guide the development of a more advanced, digitally-enabled approach going forward. The maturity model is a vendor-neutral framework designed to support the implementation and optimization of a hospital-centric wound care program. The model takes an evolutionary, staged approach to support adoption of increasingly advanced digital tools and technologies to elevate a clinical program and deliver superior clinical, operational, and economic outcomes.
In the previous entry in this series, we served an introduction to the model itself.
In this installment, we will discuss some strategies designed to help your organization progress to a higher level of maturity in digital wound care, specifically the importance of developing a well-coordinated, multidisciplinary team of clinicians working in concert to deliver comprehensive care.
Part 3 – Building a Top-Tier Wound Team
As a wound care program advances, not only does the size of the team expand, but so does the interdisciplinary nature of the team. Thus, communication, coordination and collaboration become critical to delivering high quality care.
Multiple wound care studies have reported significant improvements in clinical outcomes following the initiation of multidisciplinary wound care teams. A recent systematic review of these teams examined 33 studies, and found that in 94% of the studies, a reduction in major amputations followed the creation of a multidisciplinary team¹.
The Value of Multidisciplinary Team
Wound care is an interdisciplinary pursuit that requires meaningful collaboration. These stakeholders should be included in building an advanced wound care program and play an active role in the delivery of wound care:

Team Structure & Responsibilities: Framework for a SMART Team
Building the right team is important, but so is making sure the team operates cohesively and with established goals and objectives. A SMART Team is a good framework to consider:
SMART Teams:
| S | Specific, evidence-based tasks with clear accountability based on role. | Is there someone with clear responsibility for regular dressing changes, patient rotations or preparing for rounds? |
|---|---|---|
| M | Measurable and meaningful indicators for quality monitoring and performance of each role. | Have you established the frequency of wound assessments? Can you monitor adherence to completement of assessments? |
| A | Agreed upon protocols/policies with the input and approval of the full team. | Have your protocols and policies received input from all those who will be required to follow them? Each team member brings a unique and valuable perspective. |
| R | Regular review and refinement of best practice guidelines (BPGs). | Do you have a team and process to review and revise BPGs? Are BPGs easily accessible to team members at the point-of-care? |
| T | Time bound processes focused on efficiency and effectiveness. | Do your protocols, policies and guidelines indicate evidence-based frequency and duration of tasks? Pressure injuries, for example, can develop in a matter of days, if patients aren’t assessed frequently. |
Training and Education: Continuing Education to Upskill your Team
The high complexity, lack of formal education and shortage of wound care specialists means that training and education are imperative to building and maintaining a high performance and confident wound care team. In a study of over a hundred medical school curriculums in the US, investigators discovered only 9.2 hours of wound care education over four years². Further, there are approximately 500 wound patients for every wound specialist, which poses a challenge for building wound care capacity in an organization³.
Like with any change initiative, upfront, ongoing education and training is critical to adoption and success. Developing wound care policies and guidelines are worthless unless they are understood and adopted by your entire team. The more familiar nurses are with new or revised wound management policies, the more comfortable and efficient they will be when engaging with patients in the home. They should know that the right protocols, pathways, and technology are available to support their decision making.
A well-assembled wound team is only as good as the governance structure which manages it. In the next installment of the series, we cover governance strategies for creating and managing a high-performing, digitally-enabled wound program.
Sign up for our mailing list to get notified directly of new blog posts.
[¹] Jackson Musuuza, et al. A systematic review of multidisciplinary teams to reduce major amputations for patients with diabetic foot ulcers. Journal of Vascular Surgery. 2020.
[²] Nima P. Patel, et al. Comparison of Wound Education in Medical Schools in the United States, United Kingdom, and Germany. Eplasty. 2008.
[³] Amy Cassata. Why Every Provider Should Have Wound Care Knowledge. HomeCare. 2018. https://www.homecaremag.com/september-2018/nurse-wound-care-expert