For information on the 2026 CMS final changes for skin substitutes, visit: https://swiftmedical.com/2026-cms-changes-for-skin-substitute-reimbursement/
Centers for Medicare & Medicaid Services (CMS) have proposed significant changes to the reimbursement model for skin substitutes in 2026, marking one of the most substantial shifts in advanced wound care policy in years. The biggest change is rather than a payment that ranges by size from $200-$3,000+ per square centimeter, there will be set standard rate of $125.39. Other changes include a likely change to the application fee and a policy category shift from drug-like reimbursements (separately) to supply-like reimbursements (bundled with a procedure)1.
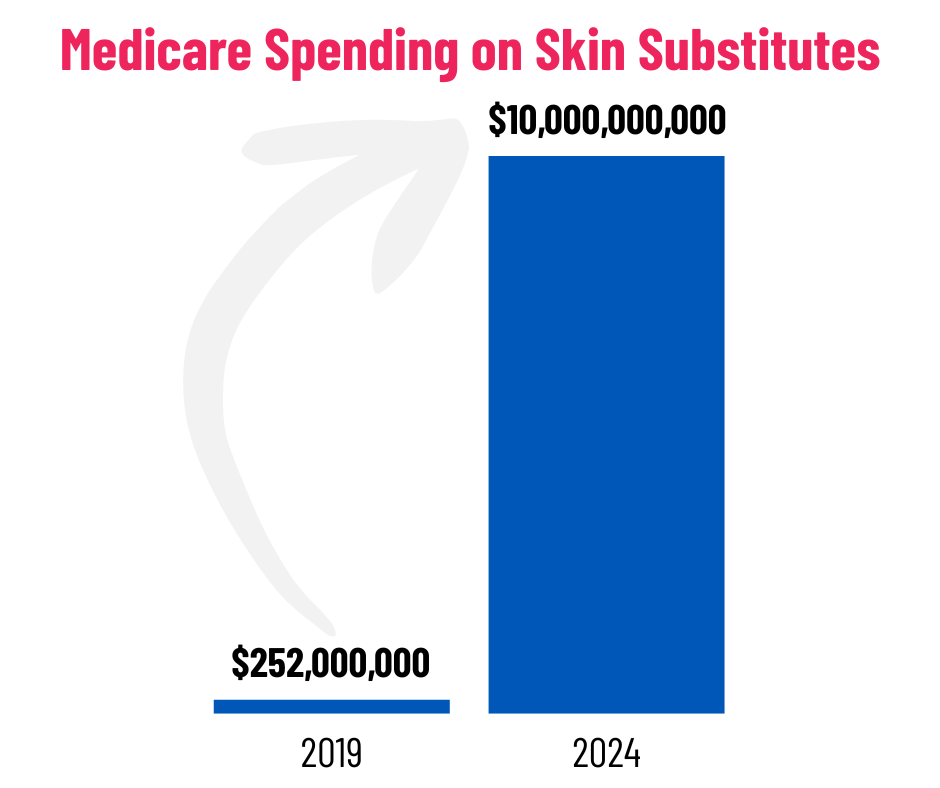
This is due to a large increase in skin substitute spending which jumped from $256M in 2019 to $10B in 20242. This new proposed change is expected to reduce Medicare spending by over 90%2. It is also expected to curb the fraud recently identified in the wound care industry by neutralizing the economic incentives that have enabled such abuse.
This is a big change in how advanced wound care is reimbursed in physician offices and may alter clinician’s financial viability, site-of-care decisions and willingness to use cell tissue-based products. The effective date is January 1, 2026 but comments are open and the changes haven’t been finalized. For wound care organizations, understanding this proposed rule and preparing for its potential clinical and financial consequences is critical.
Potential Financial Impacts
- As described above, reimbursement rates are changing to a flat national rate for all skin substitute products and all outpatient settings will be reimbursed at the same rate. As a result, providers may face decreasing margins, especially those using premium technologies.
- Practices will likely reassess product selection and billing workflows to align with the new payment structure. The policy category is currently set to change from drug-like to supply and must be billed as part of a procedure/service rather than separately.
Potential Clinical Impacts
- Standardizing the reimbursement for skin substitutes across care settings will reduce confusion and provide more stability for payment expectations.
- Pricing all skin substitutes equally could result in clinically distinct products being treated as interchangeable, potentially compromising care quality. Under the proposed rules, products with higher clinical outcomes have the opportunity for a higher value dependent upon classification and evidence. As a result, patients may experience reduced access to advanced therapies if providers opt for more financially viable options.
- Without differentiated payment, manufacturers may reduce investment in new therapies halting an area of innovation that has exploded in the last few years. With potentially lower levels of revenue for manufacturers, money spent on product innovation may be shifted to areas of higher profit.
The Critical Role of Data: Why Documentation is Your Best Defense
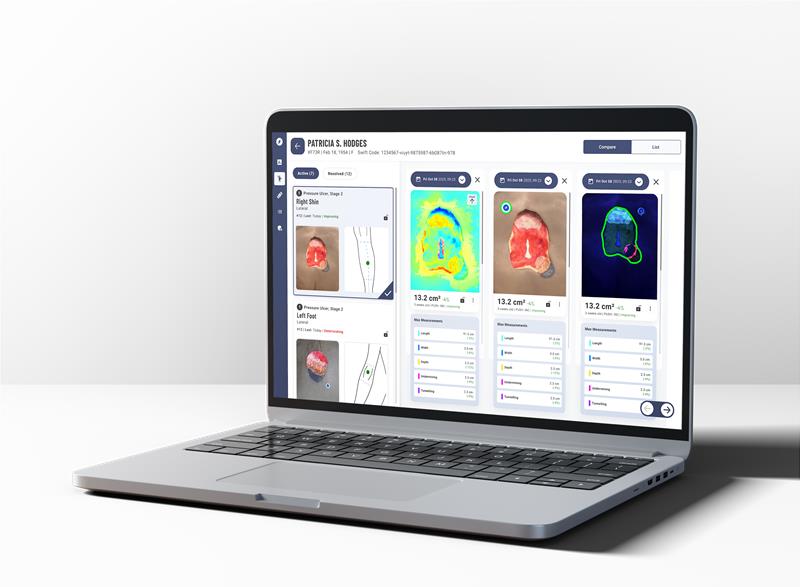
The most critical element for success under these new policies is robust, data-driven documentation. CMS is shifting toward time-and-motion studies and away from subjective survey data for valuing services3. Wound care teams must prepare for more granular documentation to back clinical decision-making especially when it comes to advanced treatments like skin substitutes. This is where Swift Medical’s digital wound care platform stands out. Our platform provides:
- Consistent Imagery: Our calibrated system provides consistent and accurate measurements and skin-tone variability allowing a seamless and repeatable visual case documentation.
- Automated Measurements: We auto-calculate and display auto wound size and depth, and depict change over time with timestamped images.
The final ruling is expected in November 2025, leaving a short window to adapt. Organizations that begin preparing now will be best positioned to mitigate financial risks and maintain high standards of patient care. Don’t wait until the new policies are finalized.
1 https://www.medpagetoday.com/practicemanagement/reimbursement/116555