The Centers for Medicare & Medicaid Services (CMS) has finalized major updates to reimbursement for skin substitutes effective January 1, 2026—a move that consolidates fragmented payment approaches into a single, site-neutral policy. These changes will impact nearly every segment of advanced wound care, from outpatient hospital departments to home health and mobile wound care providers.
The wound-care world is shifting beneath our feet. For providers operating across outpatient settings, the upcoming reimbursement changes from CMS represent both a challenge and an opportunity. The key: turning policy complexity into confident, efficient care.
The Shift
Beginning in CY 2026, CMS will reimburse many skin substitute, now classified as “wound care management” products as incident-to supplies under the Physician Fee Schedule or hospital outpatient system, rather than as high-priced biologic or drug equivalents. Historically, these products were paid under an ASP-based methodology, with costs surging recently.
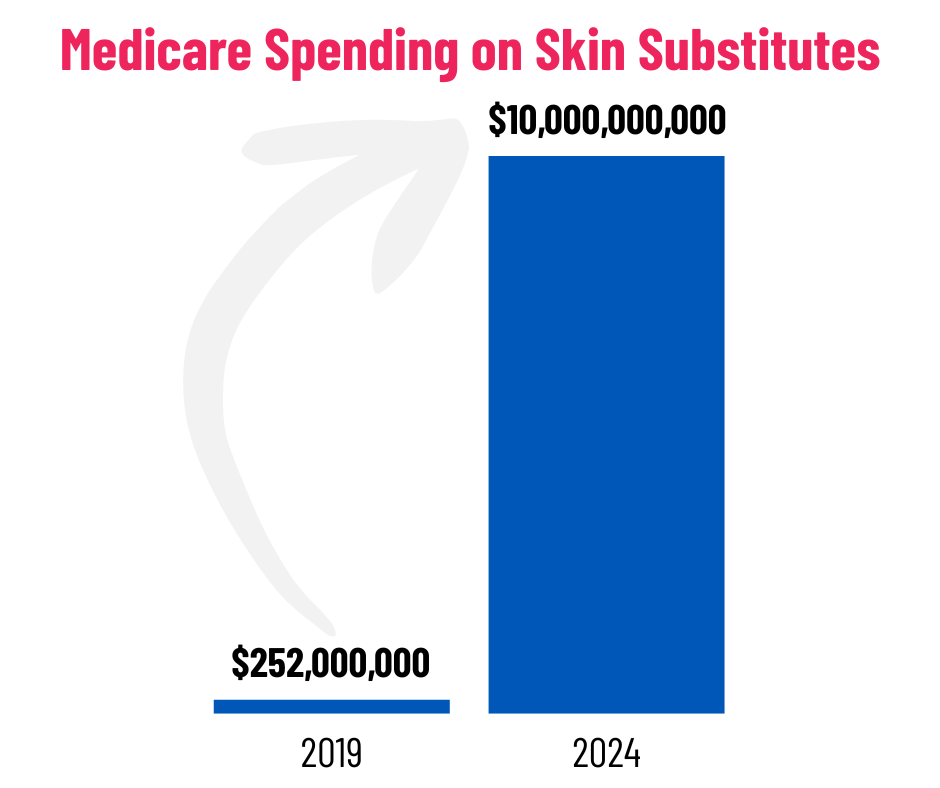
Part B spending jumped from roughly $252 million in 2019 to over $10 billion in 2024. The new rule aligns payment across sites of care (mobile, office and outpatient) and groups products by regulatory pathway (HCT/P, 510(k), PMA), aiming to encourage cost-effective innovation and responsible utilization.
On the coverage side, Local Coverage Determinations for diabetic foot ulcers and venous leg ulcers already require proof of standard-of-care failure, detailed wound assessments, and justification for repeat applications.
“Adequate clinical documentation must support the medical necessity, appropriateness, and frequency of the skin substitute application.”
~Centers for Medicare & Medicaid Services
Why Documentation Matters More Than Ever
CMS emphasized documentation as a core safeguard against overutilization and non-compliance. Providers will need to demonstrate medical necessity and appropriateness for every application, especially across outpatient wound settings, where site-neutral payment may magnify audit exposure.
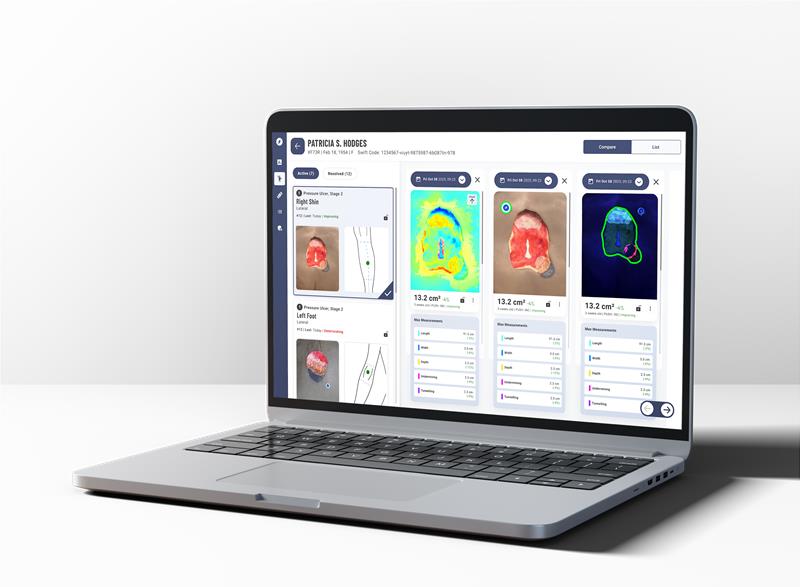
Accurate, consistent and reproducible image-based wound documentation with dashboards for progress tracking are no longer just good clinical practice, they’re financial defense.
The Ripple Effect: Market Impacts and Clinical Implications
- Providers: Expected reduction in per-application payment rates will require improved operational efficiency and precise documentation to maintain margins.
- Suppliers and Manufacturers: Pressure will mount to show cost-effectiveness and real-world healing outcomes to justify inclusion under bundled reimbursement.
- Patients: With a focus on efficiency and healing trajectory, the new rule could accelerate movement toward standardized digital documentation and remote monitoring solutions.
How Technology Can Help Providers Stay Ahead
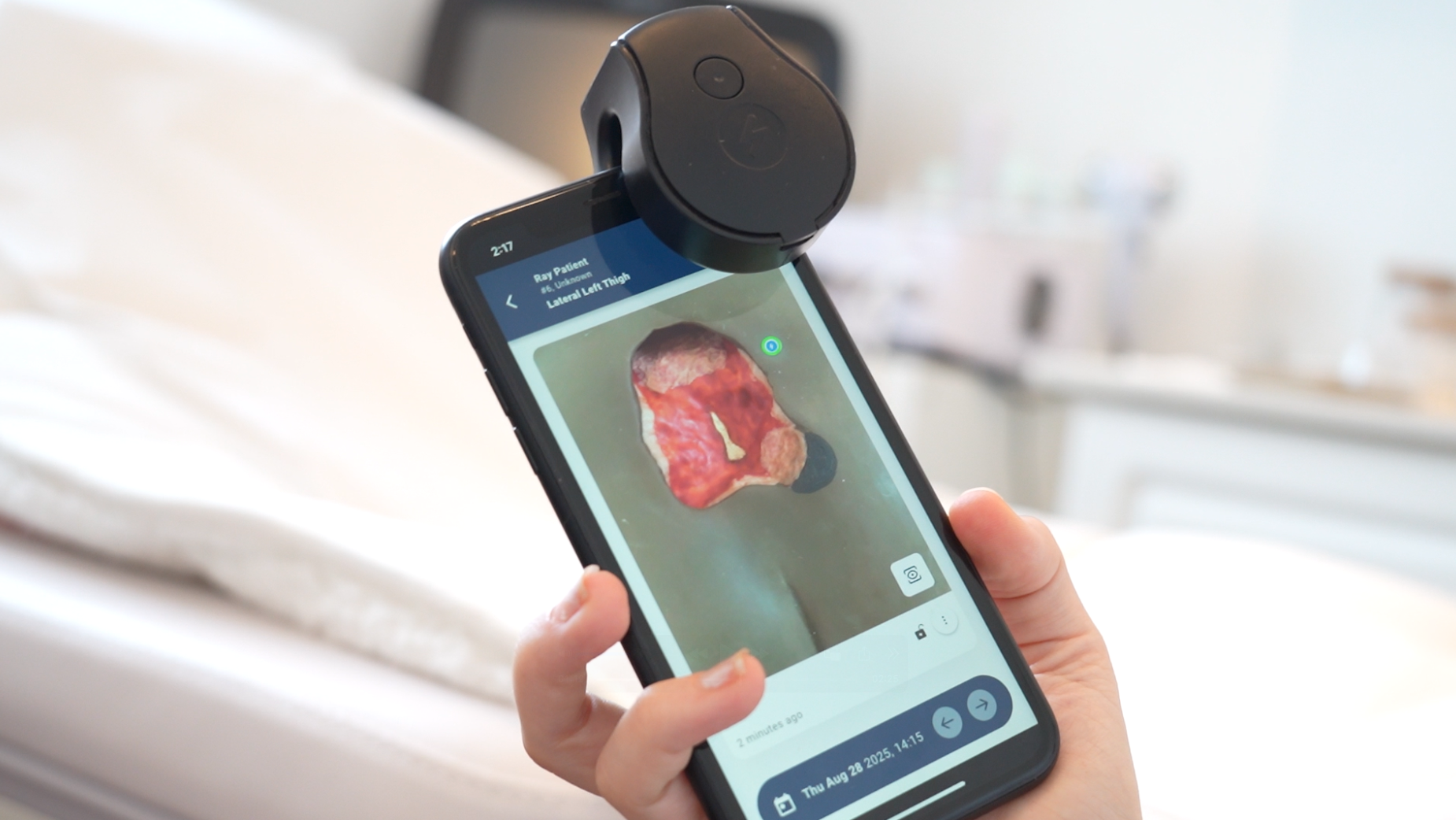
Swift Medical’s digital wound management platform—including its advanced thermal and fluorescence imaging—provides the precision, documentation, and visibility clinicians need to thrive in this new environment.
- Audit Defense: Objective imaging and structured documentation support compliant billing.
- Given heightened regulatory focus on skin substitutes (and documentation of usage, wastage, standard of care failures) tools that archive the full care episode — from conservative care trial through wound-healing outcome tracking — will strengthen providers’ compliance posture. For example, consistent documentation, image capture, and integrated analytics help create defensible records.
- Efficiency: Streamlined workflows and centralized oversight through the Swift Portal reduce administrative burden.
- Mobile or home-based wound providers especially must be lean. A technology system that integrates scheduling, image capture, measurement, reporting and billing enablement reduces administrative burden, shortens time to decision, improves throughput and supports cost-effective care delivery.
- Improved Outcomes: Earlier identification of infection and delayed healing through fluorescence and thermal data support faster, evidence-based interventions.
- Tools that capture spectral imaging (fluorescence and thermal), structured wound measurements, and pre/post treatment comparisons help satisfy the documentation demands noted by CMS. When every application of a skin substitute demands justification, clarity becomes key.
As reimbursement shifts, the value proposition for every step in the wound-care pathway is under review. Providers will need to demonstrate that interventions (including skin substitutes) are truly necessary, timely and supported by evidence. Technology platforms can embed decision-support alerts (e.g., “wound failing conservative care? Consider advanced therapy”), track key metrics (e.g., time to 50% reduction, visits to closure, cost per episode), and support internal ROI narratives.
In short, as CMS raises the bar for documentation and oversight, Swift turns complexity into confidence.
What Providers Can Do Now
CMS changes won’t wait for anyone to catch up. Providers who act now to tighten documentation, streamline operations, and modernize their wound-care workflow will be best positioned to thrive under the new payment model. This isn’t just about compliance; it’s about controlling cost, defending clinical decisions, and proving value in every episode of care.
Here’s how to prepare:
- Audit your documentation today. Review your current wound-care charts, photo capture, and clinical narratives to ensure every episode clearly supports medical necessity and wound trajectory.
- Optimize your technology stack. Confirm your imaging and wound-management tools can produce consistent, auditable records – complete with image metadata, wound dimensions, auto-depth and healing progress over time.
- Align clinical and billing teams. Educate staff on documentation expectations under the new rule, including conservative care documentation, product justification, and frequency limits.
- Track supply utilization. Establish a baseline of your current skin substitute usage and total spend per wound episode. This will be key to proving efficiency and cost savings going forward.
- Engage payers and partners early. Discuss your documentation improvements and technology adoption plans with payers, referring providers, and administrative leaders. Early collaboration can smooth coverage reviews and mitigate audit risk.
- Measure outcomes, not activity. Shift from counting procedures to tracking time-to-closure, wound-free days, and total cost of care. That’s where future reimbursement battles will be won.
Bottom line:
The new CMS framework rewards precision, consistency, and cost-conscious care, exactly where digital imaging and enterprise wound-management solutions excel. Swift’s platform is built to help providers capture complete wound data, document with confidence, and demonstrate measurable savings and improved outcomes. In short, Swift turns complexity into confidence, which is exactly what this new era demands.
What’s Next
The upcoming CMS changes aren’t about eliminating skin substitutes — they’re about reorienting wound care toward value, documentation, and outcome-driven care. For providers, this is a call to assess readiness and modernize how care is delivered and documented.
Now is the time to:
- Evaluate documentation quality and image consistency. Ensure your records clearly demonstrate medical necessity and wound trajectory.
- Standardize workflows across clinical settings to eliminate variability and strengthen compliance.
- Implement digital platforms that align with CMS’s wound management framework and support efficient, audit-ready documentation.
The reimbursement landscape may be tightening, but it’s also creating opportunity. Providers who adopt the right technology and processes now can get ahead of the curve by delivering better care, stronger documentation, and greater financial stability.
At Swift, we believe in empowering wound care teams with technology that turns complexity into confidence. If your organization is preparing for the new reimbursement environment, now is the time to act; streamline your workflows, fortify your documentation, and lead the transition to value-based wound care.
Swift gives your team the tools to do exactly that — transforming every image, every visit, and every record into measurable confidence.
See how Swift can help your organization prepare for the 2026 CMS changes.