According to the Agency for Healthcare Research and Quality, more than 17,000 lawsuits related to pressure injuries are filed annually in the United States, second only to wrongful death lawsuits.
Being sued creates significant discomfort for all involved, including caregiver and employer. Irrespective of the time, resource, and financial implications, there is a significant personal toll. Who likes their ability, credibility, and caring nature to be questioned? Fairly or unfairly, it’s not a pleasant experience when challenged by a lawyer, some of whom make a living “chasing wounds.”
One of the biggest pain points when it comes to litigation is the collection of documentation needed for the court case. With the best practices in prevention and care in place, skilled nursing facilities can often avoid litigation altogether. However, if your facility does come under scrutiny in court, the quality and completeness of your wound program’s documentation is a crucial factor in determining the outcome of any case.
The Centers for Medicare & Medicaid Services have acknowledged that some pressure injuries are unavoidable, which means they can occur despite receiving the best care possible. However, it’s up to the facility to prove they did everything they could to manage and prevent the wound, and despite that, the patient still developed that pressure injury.
When you identify an unavoidable pressure injury your responsibility moves from avoidance to management. The fact that it is unavoidable does not remove the need for best practice. Indeed your responsibility in ensuring the best care for your patient and their pressure injury is more important than ever. But unless there are clear documentation protocols in place, it can be difficult to prove that best practices were followed and an appropriate standard of care was delivered.
Documentation and Burnout
A major challenge clinicians face when documenting wounds is competing priorities and time pressures. Staff in skilled nursing facilities are busier than ever with new challenges to manage from the COVID-19 pandemic. Some facilities also struggle to incorporate technology into their clinical workflows as a result of using multiple unintegrated systems. A major contributing factor to nurse burnout is the burden imposed by duplicate documentation across numerous information systems and EHRs.
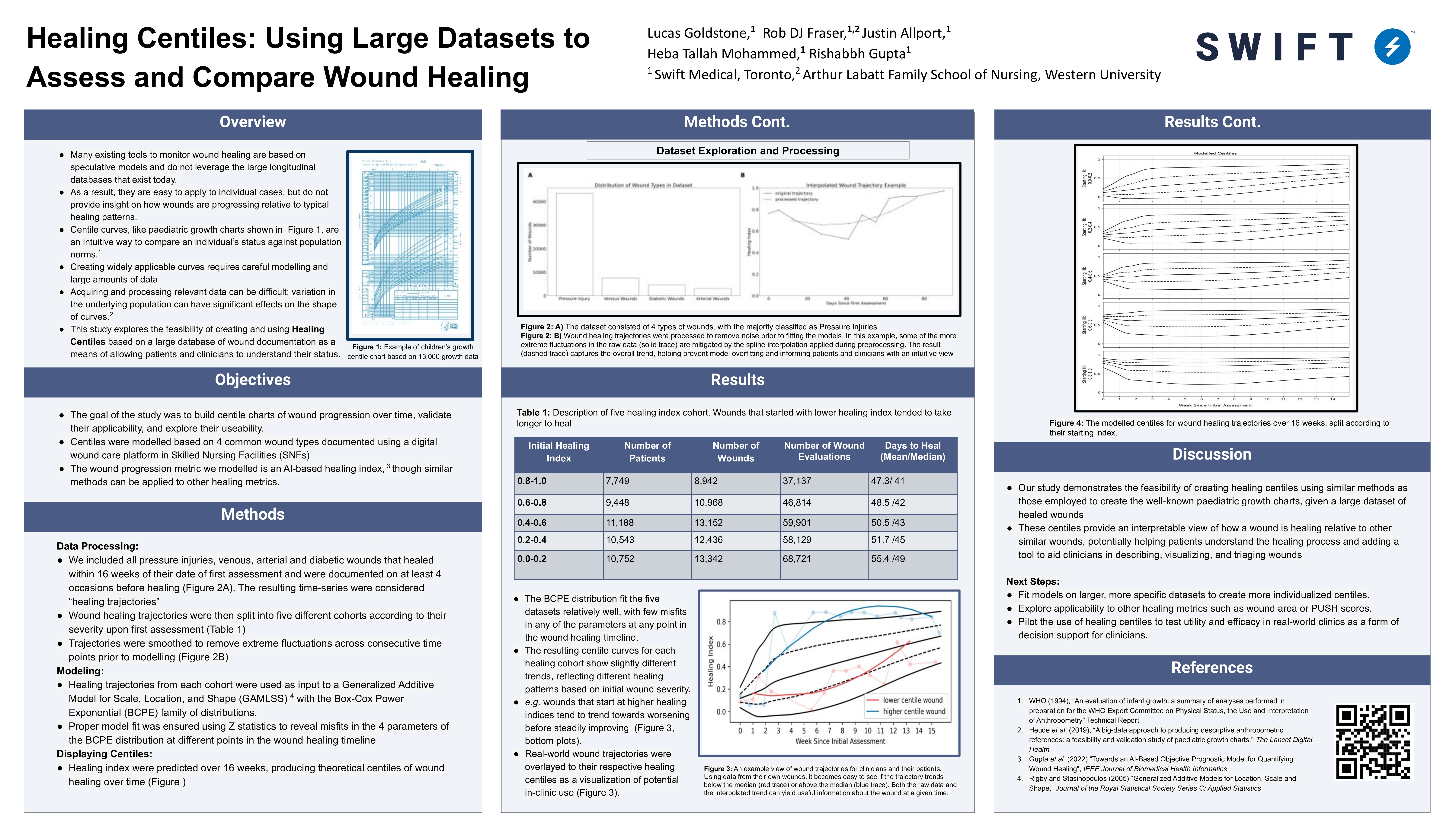
Swift has designed our wound management platform with deep empathy for the end user to make documenting wounds easy and intuitive. Because our technology is integrated with many of the leading EHRs in the skilled nursing sector, evaluations and images captured using Swift are easily stored in other digital systems used across the facility. The Swift Skin and Wound app can deliver best practices to the clinician at the point of care, and ensure that all relevant information about the wound is correctly documented in order to make informed decisions around treatments.
It’s crucial that administrators have oversight into all wounds at their facility in order to provide the standard of care required to avoid litigation.The Swift Wound Dashboard provides visibility into all wounds and can be filtered by location, wound type and when they were acquired. Staff can quickly see which wounds are deteriorating and which are improving. This allows staff to direct limited wound care resources to those that need it the most.

It’s as easy as selecting the patient and picking the date range of the needed documentation. With a simple click of the button, it’s all exported into PDFs which can be printed and are admissible in court. What can take days for already overworked clinical staff to dig out, copy, and assemble can be done within minutes.
To see how Swift can help improve documentation challenges at your organization, click here to book a demo today.