Welcome to Swift Medical’s multi-part series on the new Home Health Value-Based Purchasing Model.
Feeling unsure about what impact the upcoming Home Health Value Based Purchasing Model (HHVBP) will have on your organization? You’re not alone. A recent survey by Home Health Care News found that 63% of home health providers were unsure or indifferent about the impact it has made on their organizations thus far. And yet despite this, 42% of respondents believe that value-based contracts will account for more than half or most of their organization’s revenue in the next 3-5 years.
In the first entry in this series, we provided an easy to understand introduction into how the new model will operate. In this entry, we will discuss the crucial role wound care plays in reducing hospitalizations, the most heavily weighted quality measure under value-based purchasing.
Wounds: The #1 Reason for Hospitalizations in Home Health
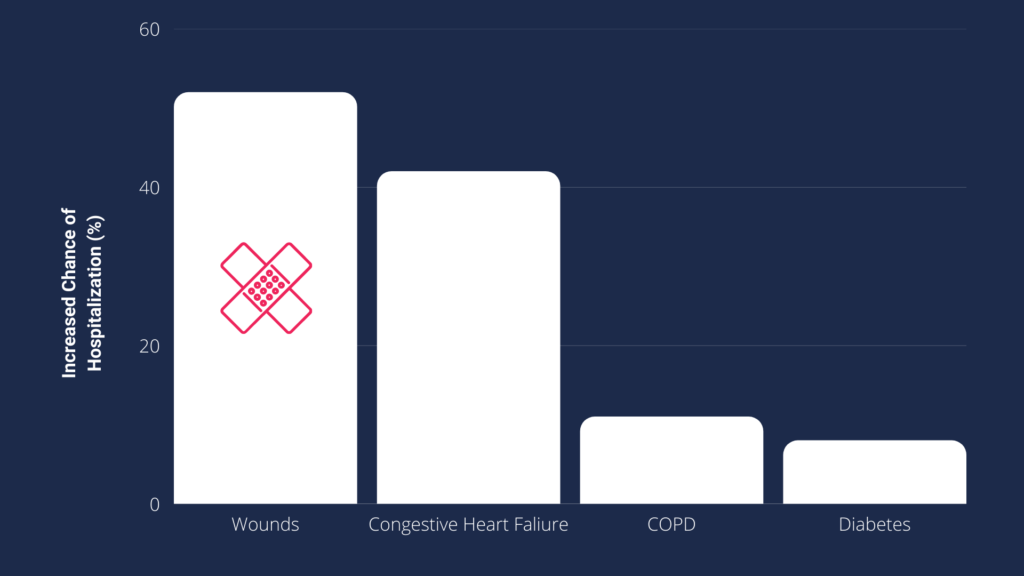
Unplanned hospitalizations are a challenge for all home health agencies across the country. Any time a patient is sent to hospital when receiving care in the community, something has gone wrong. These events are associated with poor clinical outcomes and cost the health care system upwards of $17B annually according to the Agency for Healthcare Research and Quality. However, typical fee-for-service payment models do not incentivize providers to prevent these episodes in the same way as value-based payment models can. Because of their enormous cost to the healthcare system, the new HHVBP model weighs unintended hospital use more heavily than any other quality indicator. This means that starting in 2025, home health agencies across the country will have their medicare fee-for-service payments adjusted ±5% based on their ability to reduce hospitalizations more than any other factor (35% of total weighting). It is then no surprise that in the 9 test states that have piloted value-based purchasing, hospitalizations was the area that experienced the greatest year-over-year change, improving at a rate 2x that of any other measure. This makes hospitalizations the most competitive quality measure. If your organization cannot improve your hospitalizations at a rate that outpaces your competitors, you could be vulnerable to a poor score in this area–increasing likelihood of a negative payment adjustment.
And just as hospitalizations are the number one metric that will impact HHVBP payment adjustments, wounds are the number one factor that contributes to hospitalizations in home health. Patients with wounds have a 52% increased risk of hospitalization in home health (more than any other diagnosis or factor). With roughly 1 in 3 home health patients having at least one wound, anything done to improve the quality of your wound program can have a significant impact on your organization’s performance under HHVBP.
Improved Healing Rates with Digital Wound Care

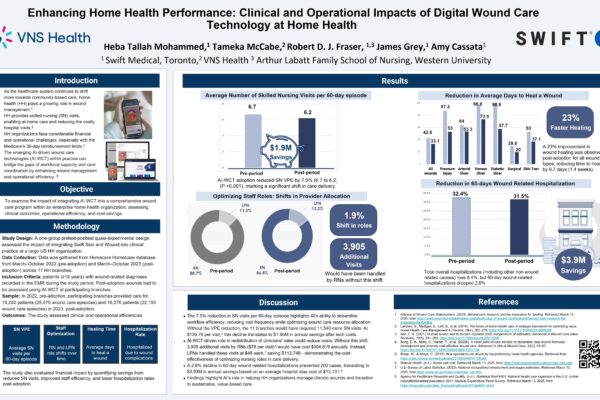
Swift Medical’s digital wound platform provides a proven solution for improving both the clinical and financial performance of your organization’s wound program. A multi-state home health agency that adopted Swift saw increased standardization of care, adherence with best practices, and accuracy of wound measurement, which resulted in up to 70% improved healing rates across several wound types. When wounds heal faster the risk of infection or other complications is significantly reduce which in turn helps to keep patients at home and avoid hospitalizations.
Improved Surveillance

Swift Medical’s digital wound platform not only improves the experience for the nurse at the point of care, it also provides a level of insight into the progress and risk status of your wound population via our configurable dashboards. With greater insight into your wound patient’s needs, you can make informed decisions about where to allocate staff and proactively intervene for patients at-risk of hospitalization.
Improved Performance
With improved healing rates, surveillance, and risk-management, organizations that have adopted Swift have seen upwards of a 13% reduction in hospitalizations post-implementation. And because we have designed our technology for usability, it is easy to train staff and deploy across your organization. Swift customers usually see measurable improvements in as little as 6 months. With just six months until the first HHVBP performance year in 2023, there is still time to implement Swift and improve your organization’s hospitalization rate and set yourself up for success under the new model.
In the next entry in this series we will go into more detail about how Swift can help improve your patient satisfaction, another key quality measure so that your agency can thrive under HHVBP.
Our latest webinar with Maxwell Healthcare Associates provides a better understanding of how your agency can thrive under the value-based purchasing model by adopting digital wound tools that help:
- Reduce rehospitalizations;
- Improve the quality of care, and;
- Enhance patient and provider satisfaction.