Proper management of wounds in skilled nursing facilities is crucial to an organization’s overall success. The consequences of a poorly managed wound care program can be devastating. In the skilled nursing sector, 87% of litigation is settled in favor of the plaintiff. The cost of these lawsuits can be astronomical, with the median settlement in excess of $1,000,000 for cases involving a pressure injury, the most common form of wound-related litigation¹.
Measurement is perhaps the most central component of treatment and management in wound care. Accurately and consistently capturing wound measurements over time is crucial for understanding whether a wound is healing. Conversely, the inability to understand changing wound dimensions can result in inappropriate care decisions, adverse patient outcomes, and unnecessary costs. Regularly measuring a patient’s wound is essential to knowing if the wound is getting smaller or larger which ultimately determines if the wound is getting better or worse, and whether or not it is responding to treatment.
Common Barriers to Consistent Wound Measurement
- The Problem with Paper: Accurately assessing if a wound is getting larger or smaller can be difficult using the most common method for wound measurement today: the paper ruler. Popular because of their low cost, these unsterile paper rulers have been shown to overestimate the actual wound area by more than 40%.² Additionally, wounds are rarely a standard geometric shape. Wounds with irregular shapes or those that curve around the body can be even more difficult to measure using a paper ruler.
- Different Care Providers: Patients often have multiple care providers and each individual clinician taking a measurement could use different techniques and may have varying levels of experience in wound management. Using measurement methods that result in subjective measurements can create added variability and reduce the consistency. This can make it even harder to accurately determine if a wound is healing properly.
- Depth Discomfort: In addition to measuring the length and width of a wound, measuring the wound’s volume is also essential in determining if a wound is getting smaller or larger. The traditional method for measuring wound depth is with a cotton-tipped applicator. This method is error-prone, as different levels of pressure applied while measuring can provide inconsistent results. Worse still, probing a wound can be extremely painful for patients.
Augment your Accuracy with Swift
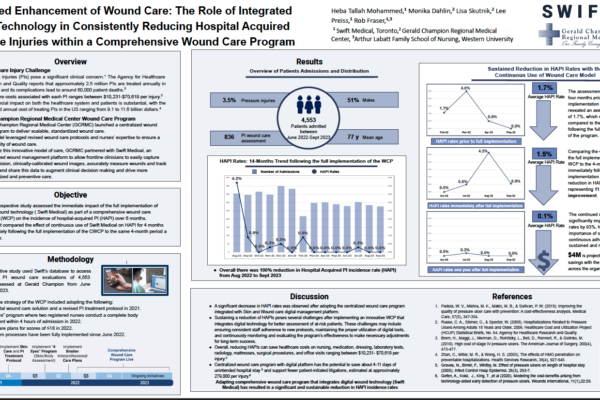
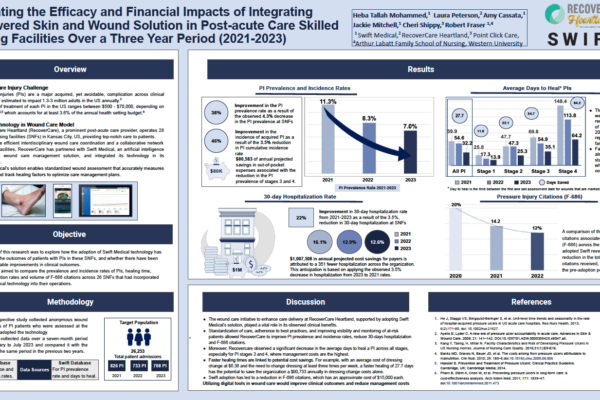
Deploying Swift Skin and Wound as part of your organization’s wound care strategy can help improve the accuracy and consistency of wound measurements by leveraging our advanced machine visioning technology and easy-to-use digital workflows.
- Digital Precision: Swift Skin and Wound displayed 95%+³ inter-rater reliability in a peer-reviewed study, a significant improvement over traditional paper ruler measurement methods. And because Swift’s technology is easy to use, even care providers with limited experience in wound care can feel confident about the accuracy of their measurements.
- Digital Documentation: Overcome the challenges associated with multiple care providers with Swift’s centralized digital document management that makes assessments, images, and notes available across your entire organization in real time.
- Digital Depth: Swift Skin and Wound’s AutoDepth feature allows clinicians to accurately measure the depth of a wound within 2mm using our proprietary machine visioning technology, all without the discomfort of physically probing a wound.
Swift is here to help skilled nursing organizations who are ready to dramatically improve the accuracy and consistency of their wound measurements with our industry-leading technology.
Contact us today for a demo and to find out how we can help transform your wound care program.
¹ Voss, A. C. et al. Long-term care liability for pressure ulcers. J. Am. Geriatr. Soc. 53, 1587–92 (2005).
² Angela Christine Chang, et al.. A Comparison of Wound Area Measurement Techniques: Visitrak Versus Photography. ePlasty Web. 2014, 2011. + Louis D. Photographing pressure ulcers to enhance documentation. Decubitus. 1992.
³ Wang SC, Anderson JAE, Evans R, Woo K, Beland B, Sasseville D, Moreau L. Point-of-care wound visioning technology: Reproducibility and accuracy of a wound measurement app. PLoS One. 2017 Aug 17;12(8):e0183139.