
Skilled Nursing Facilities
Clinically validated touch-less wound measurements with standardized documentation

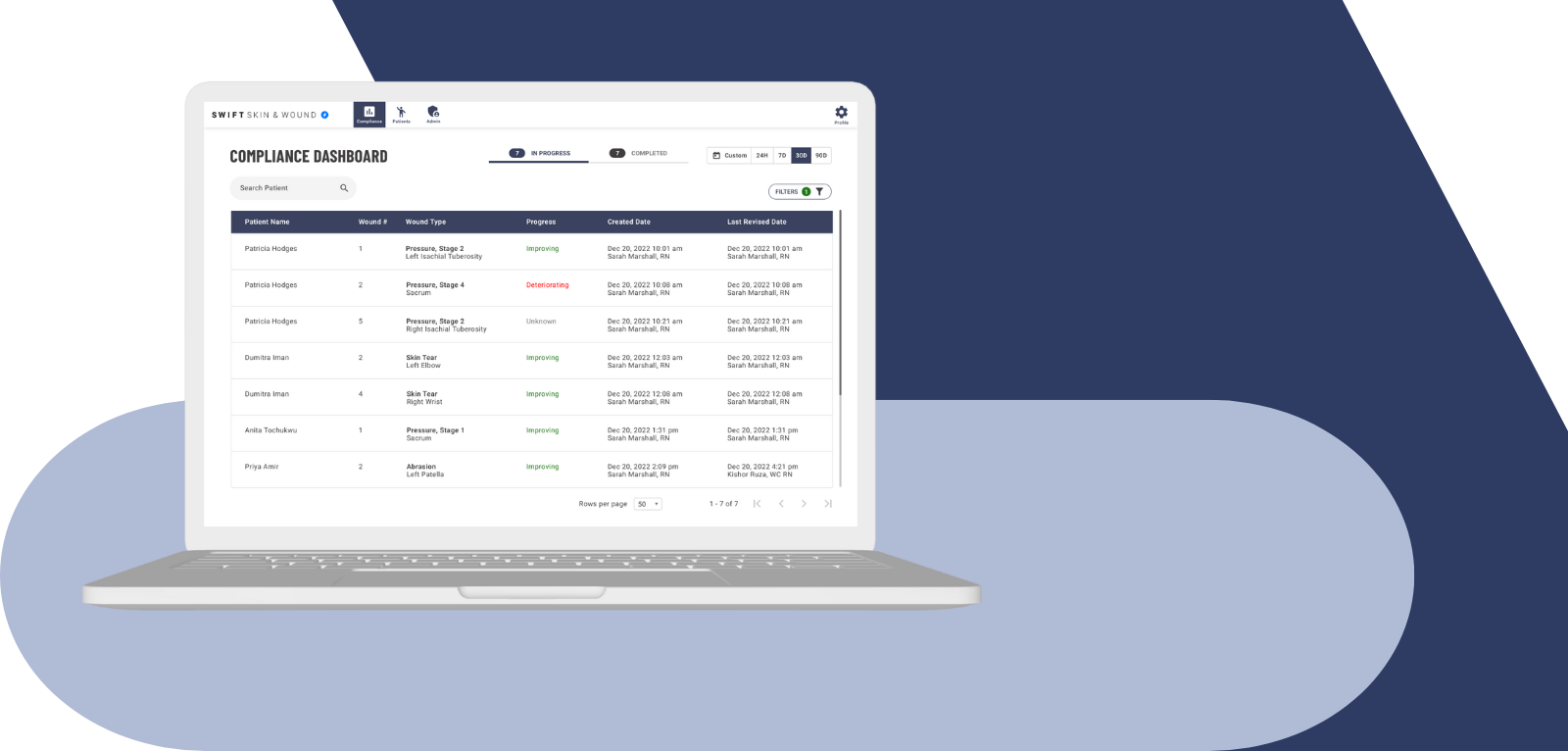
Comprehensive documentation for interdisciplinary teams
Swift Skin & Wound™ ensures consistency of documentation for all users. Interdisciplinary teams can have complete visibility over the entire wound care process in single or multi-facility organizations. Identify the current status of a wound’s healing progress, conduct analysis and provide outcomes data.
Swift Skin & Wound™ helps you get ahead identifying high risk patients and ensuring the proper treatments and plans are in place. Swift’s comprehensive wound evaluation meets all federal and state regulations.
Reduce legal risk and improve regulatory compliance
Swift Skin & Wound™ provides a system to collect and manage the proper clinical and regulatory documentation of skin and wound evaluations so you’re in compliance with clinical regulations and best practices.
Clients have used the clinical data and reports contained within Swift to successfully ward off claims and litigation.
Proactively monitor at-risk patients and rapidly react to new or worsening wounds
Reduce the prevalence of wounds by 43% through real-time monitoring of high-risk patients, accurate and consistent wound assessments, and the availability of treatment best practices at the fingertips of clinicians.

