Welcome to Swift Medical’s Multi-part Staffing Optimization Series for home health.
We know that high-performing home health agencies depend first and foremost on high-performing people. And as many studies have shown, staff that feel supported, fulfilled, and satisfied in their work perform better and have lower turnover. This series will explore various topics in the sector regarding staffing, including improving recruitment and retention, visit utilization, and empowering clinicians to practice at the top of their license.
In this installment, we will discuss how to manage referral growth and reduce the amount of rejected referrals, with a particular focus on wound care patients.
The past two years have been tough for home health agencies. The major regulatory changes of PDGM coinciding with a once in a lifetime pandemic has created unique challenges for the home health sector.
One of the biggest impacts of COVID-19 has been its effect on staffing levels. A recent survey found that 3 in 10 frontline healthcare workers considered leaving their job because of increased risks and stress during the pandemic.
The result is that home health agencies have struggled with capacity challenges as more and more organizations have seen themselves turn down referrals from acute care settings because they lack the staff to care for additional patients.
In the first month of 2022, home health agencies rejected 58% of referrals from hospitals, according to analysis from CarePort, a Wellsky Company.
“The biggest thing for us is that the volumes are there, but the staffing has been the challenge,” said Barb Jacobsmeyer, CEO of Encompass Health’s home health and hospice segment, during an earnings call in early 2022. Encompass reported that the company lost a “minimum” of 1,700 home health admissions during the last quarter of 2021 due to staffing constraints.
Considering the significant challenges facing home health agencies, it is understandable that some may want to avoid the added burden of wound patient referrals. Wound patients commonly deal with complex, comorbid conditions and require resource intensive care, from both a staffing and supplies perspective. Access to specialized wound experts can be hard to come by; in the United States, there is only one wound specialist for every 500 wounds. Recognizing this, the CMS has decided to reward the home health agencies that take on this vulnerable, clinically complex patient population. Out of the 12 clinical groupings under PDGM, wounds present the highest potential reimbursement opportunity. Further, at a national level, wound episodes have experienced the largest total increase in reimbursement (when compared to the former PPS structure), with an increase of nearly $350M (up 23.7%).
Increasing your Wound Program’s Capacity with Swift
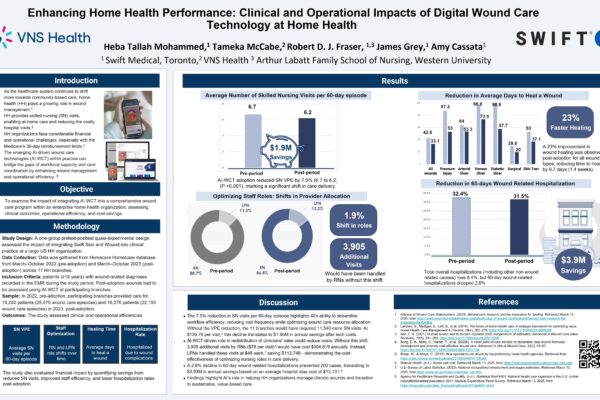
Swift Medical’s digital platform is designed to enhance the ability of home health agencies to better manage complex wound patients. With access to realtime information about the healing status of your wound patients, leadership can better allocate scarce staffing resources to proactively intervene and manage those most at-risk. With our technology, you can ensure the most appropriate nurse completes each in-person visit, while providing virtual support from the rest of the wound care team. By having more specialized wound nurses support visits remotely, you can have confidence that wound experts are being used to their full potential at a time when staffing levels are a key concern. The best part is that efficiency is not coming at the expense of quality. Home Health agencies that implemented Swift have seen a 70% improvement in wound healing rate and a 13.5% reduction in re-hospitalizations.
Reject Fewer Referrals Today, Grow More Referrals Tomorrow
The unique circumstances of the pandemic might mean that even the most efficient home health agencies are still forced to turn down some referrals. However, investing in technology that empowers your staff to manage more complex patients more efficiently can help you turn down less referrals while accepting a higher proportion of potentially more profitable wound referrals.
As the pandemic’s impact on staffing wanes, agencies that have established their ability to effectively manage wound referrals will be best positioned to grow their business. By showing your institutional referral partners that you can still accept complex wound patients at a time when the home health industry as a whole is rejecting referrals at its highest ever rate will help you build credibility and confidence. And since Swift also enables you to maintain and improve key patient outcomes, like re-hospitalizations, your partners will have even more reason to send you referrals in the future.
Home health agencies that implemented Swift have a proven record of successfully growing their wound patient referrals. Reach Healthcare Services, a leading Texas-based, registered nurse-owned and operated home health agency grew the size of their wound care program by 17% through increased referrals after implementing Swift’s technology. With the right tools in place to support your team, you can have the confidence to accept more referrals from institutional partners and establish your agency as an innovator during this challenging time for the industry.

To learn more about building a profitable wound care program in the PDGM era, download our ebook here. And to see Swift’s industry leading, AI-powered computer visioning and analytics technology in action book a demo today.
To get notified directly when the next installment in the Staffing Optimization series is here, sign up below.