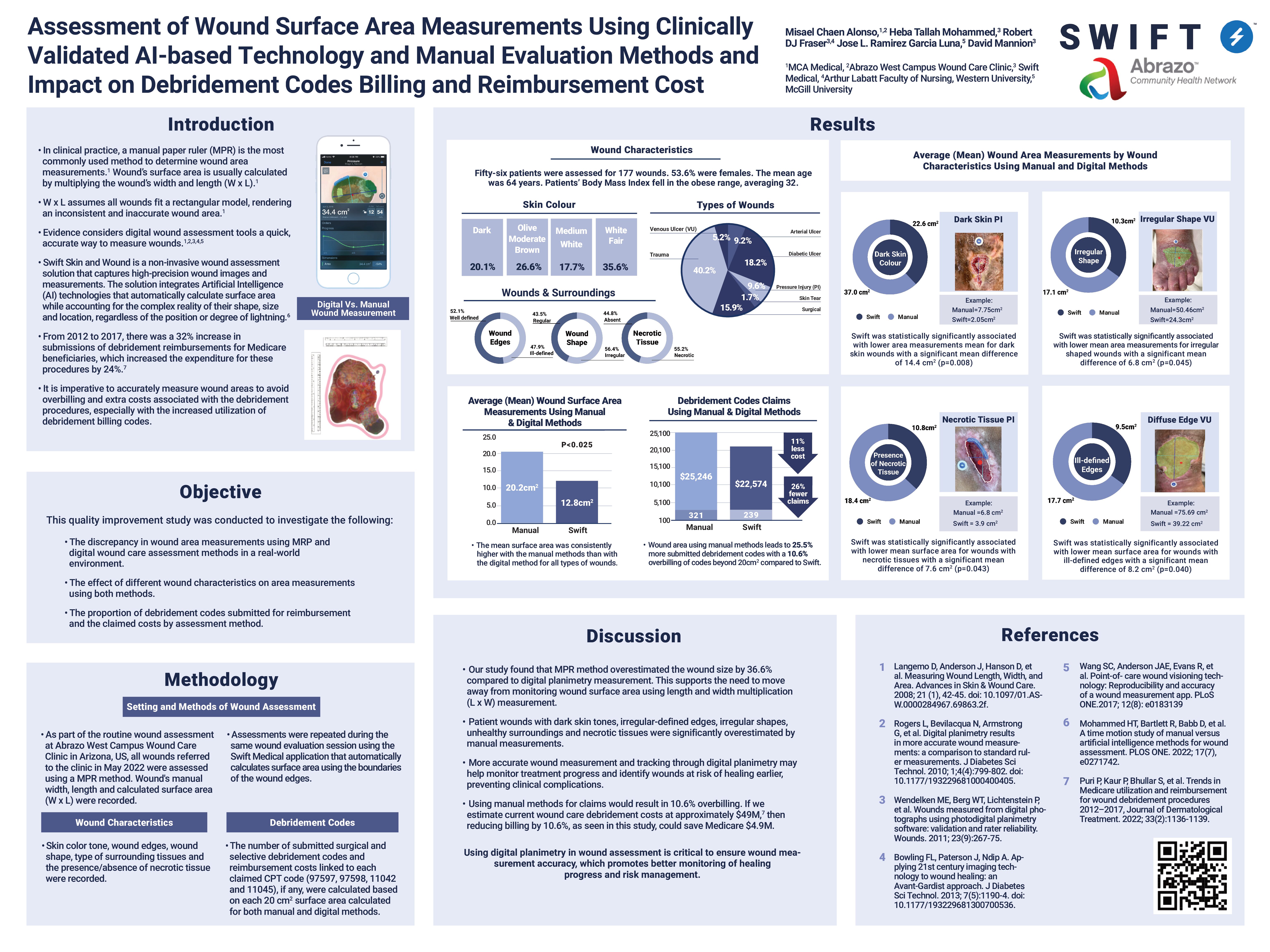
Authors: Misael Chaen Alonso, Heba Tellah Mohammed, Robert D J Fraser, Jose L Ramirez Gracia Luna, David Mannion
Objectives: Many studies addressed the inaccuracy of the manual paper-ruler method in calculating wound surface area as it assumes a rectilinear shape of all wounds, which is not the case. This quality improvement study:
- Investigated the discrepancy in wound area measurements and the associated factors using Swift wound care application vs. traditional paper ruler method in a real-world environment.
- Compared the proportion of debridement codes submitted for reimbursement and associated billing costs by the assessment method.
Methods: In May 2022, Swift collaborated with a physician at Abrazo West Campus Wound Care Clinic. The wound care physician assessed and recorded the width and length of the same 177 wounds of 56 patients using Swift and manual paper-ruler methods.
Swift automatically calculated the wound area measurement using the traced wound dimensions. As for the manual method, the width X length formula was used to calculate wound areas for the same wounds. The total cost of the wound care debridement was calculated for both methods using the reported CPT® of four different types of billing codes based on 20 cm2.
Results: The mean surface area was consistently and significantly higher with the manual methods than with the digital method for all types of wounds. Overall, the manual area measurements overestimated the wound area more than digital applications by 36.6%.
Overestimation of wound area measurements using the paper-ruler method was associated with dark skin tone wounds, irregular-defined edges, irregular shapes, unhealthy surroundings and necrotic tissues. For example, manual methods calculated a larger wound area for wounds with dark skin tone compared to the digital wound assessment tool (Swift) by 63%. and by 70% for wounds with necrotic tissues.
Analysis of billing codes in this study identified that manual methods led to 25.5% more debridement codes being submitted and an overbilling of 10.6%.
Conclusion: Accurate surface area tracking can serve as a better indicator of treatment efficiency and support modification of treatment plans. Precise measurements can be used for better risk management and prognostics. Using digital planimetry to ensure accuracy of wound measurement is critical to promoting superior patient outcomes, clinician experience, and health system sustainability.
To learn more about the research conducted in this poster, or to speak with the Swift Medical team about digital wound care, request a demo below.