Measurement is the basis for diagnosis, treatment and management in wound care. The ability to accurately and consistently capture wound measurements over time, and thus understand wound is healing, leads to evidence-based, high quality care. Conversely, the inability to understand changing wound dimensions can result in inappropriate care decisions, adverse patient outcomes and unnecessary costs.
Why Ongoing, Consistent Wound Measurement is So Important
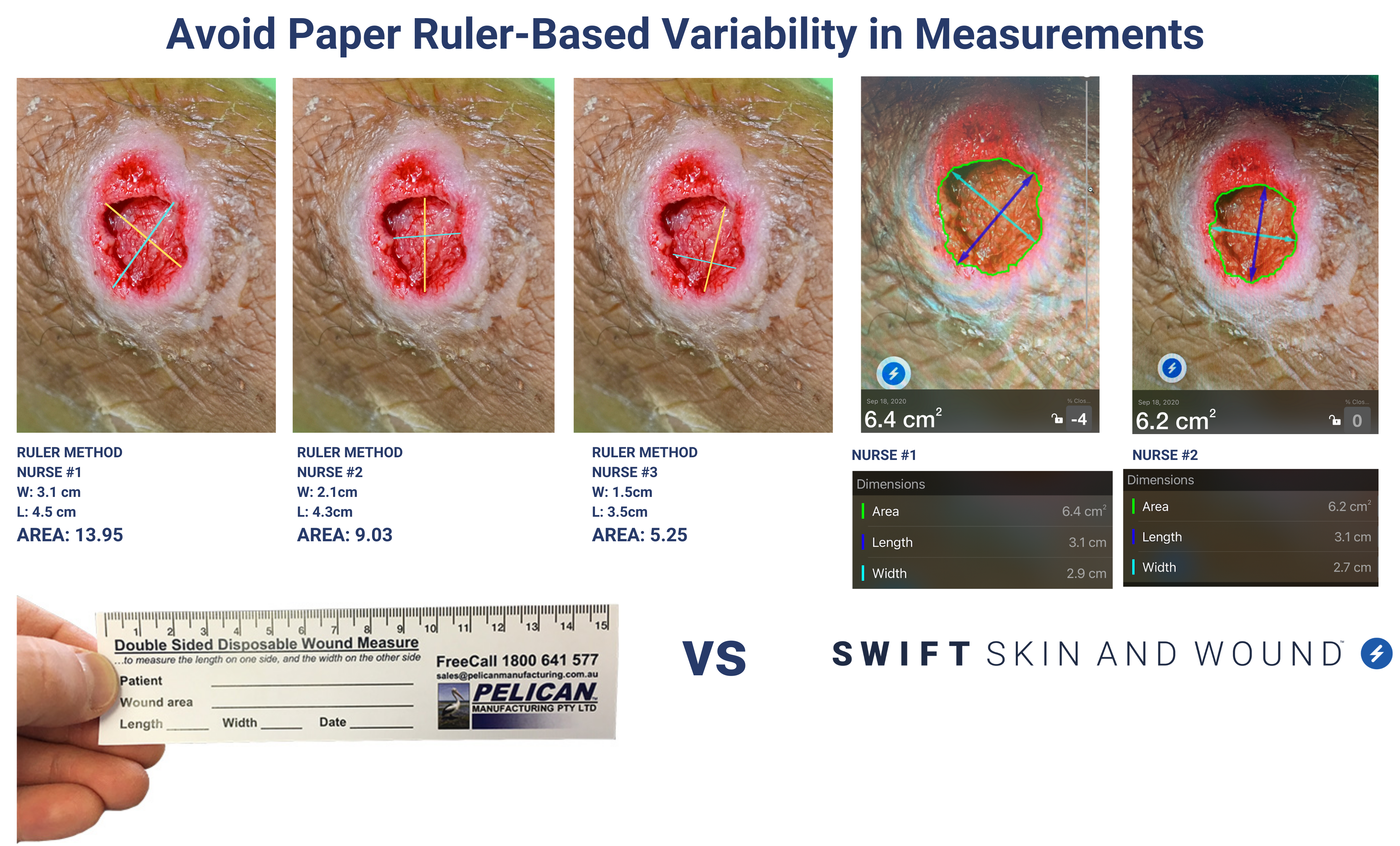
Consistent wound measurements are critical to understanding and managing wound healing over time. By regularly measuring a patient’s wound, care providers can determine if the wound is getting smaller or larger – essentially, if the wound is getting better or worse, and whether it is responding to treatment or not. Accurately assessing if a wound is getting larger or smaller can be quite difficult to determine with many current measurement methods, such as with a paper ruler. Irregular shaped wounds can be difficult enough to measure accurately once, by one clinician, nevermind measured consistently across numerous assessments, by numerous clinicians, in numerous environments – which can drastically compromise measurement consistency.
This is important because tracking wound progress impacts:
- Quality of Care: Evaluating wound healing allows care providers to recognize if a wound is not healing as expected and modify the patient’s plan of care to avoid complications, such as hospitalization, infection and amputation.
- Cost Management: Wound care is a resource-intensive discipline, and the cost of delivering care can quickly surpass the potential reimbursement if wounds are not appropriately monitored. Without the ability to recognize deterioration, worsening wounds without proactive treatment can lead to additional costs associated with health complications and prolonged care.
- Resource Planning: Insights into wound healing progress allow care providers to more accurately predict how long it will take a wound to heal and properly allocate resources to best care for that patient – supporting broader organizational staffing and supply management.
The Challenges with Achieving Consistent Wound Measurements
While consistent wound measurements are critical to best practice wound care, it remains a challenge for many healthcare organizations – impacting the quality and cost of wound care delivery. Some of these challenges include:
- Different Care Providers: Patients often have multiple care providers and each individual clinician taking a measurement could use different techniques or tools and could have varying levels of experience in wound management, resulting in variations from measurement to measurement.
- Wound Shape: Wounds are seldom geometrical, and wounds with irregular shapes or those that curve around the body are very difficult to measure.
- Various Methods and Tools: Many organizations have different practices and methods for measuring wounds, using solutions of varying effectiveness, from paper rulers to digital cameras to mobile software applications.
- Multiple Care Environments: As patients often receive care across multiple care settings, such as a community clinic, a hospital and their own home, different environmental factors, such as lighting, can result in inconsistent and unreliable wound measurements.
- Broad Clinician Expertise: As the average physician receives only 9 hours of wound didactic during medical school, a lack of competence or confidence in wound management could mean inaccurate and inconsistent measurements.
The Evolution of Wound Measurement
Technological innovation has led to significant improvements in the accuracy and consistency of wound measurements. Recent advances in digital wound care have made it possible to overcome many of the challenges described above. State-of-the-art, mobile applications with sophisticated AI and visioning capabilities can now automatically capture and calculate wound dimensions – including length, width, depth, perimeter and surface area – with sub-millimeter accuracy.
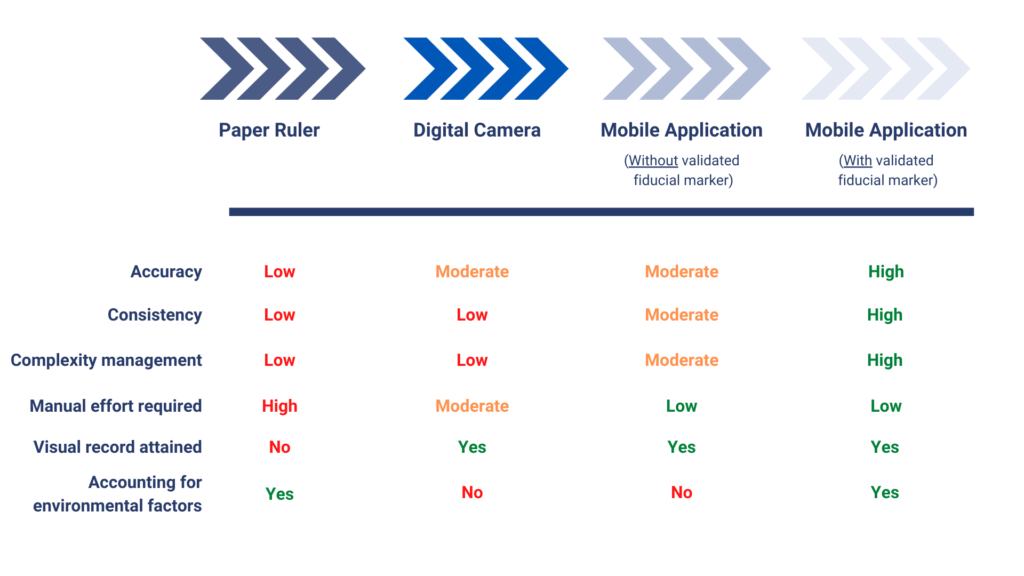
Most healthcare organizations that care for wound patients use one of these solutions to complete wound assessments: a paper ruler, a digital camera or a digital software application. With each successive innovation or approach, the reliability of wound measurements has improved – and with it, the quality of wound care.
Ages of Innovation in Wound Care Measurement
Age I: Paper Ruler
- Studies have shown wound are calculations using LxW manual ruler method can overestimate area by 44%.
- Less effective at measuring irregular shaped wounds or ones that wrap around the body, making true surface area difficult to calculate.
Age II: Digital Camera
- More accurate than the ruler method, but still a manual process that uses ruler-based measurements.
- Measuring a wound from an uploaded digital photo is time-consuming and costly due to the manual analysis and filing of each photo in the patient record.
Age III: Mobile Application (without registered fiducial marker)
- Automated measurements are more accurate than previous methods, but without a validated fiducial marker the application cannot appropriately account for environmental factors that can compromise consistency between wound images.
- Numerous hard-to-control factors that can distort wound measurements include variations in lighting, the difference in the angle a photo is taken or the distance at which a photo is taken.
Age IV: Mobile Application (with registered fiducial marker)
- Most accurate and consistent wound measurements technology on the market – demonstrated in peer-reviewed clinical trial and registered by the FDA and Health Canada.
- The controlled manufacturing process and supply chain for fiducial markers means the calibrant is a consistent size and color, which in turn means wound photos are also consistently calibrated for size and color.
- Both measurement consistency and accuracy demonstrated above 95%.
The State-of-the-Art Wound Measurement Technology
Swift Skin and Wound is a clinically validated wound management solution with advanced, AI-powered visioning capabilities. This technology fits in Age IV of the wound care innovation spectrum, as it uses HealX, a FDA-registered fiducial marker, to enhance the accuracy and consistency of wound measurements under changing environments between wound assessments.
As published in a peer-reviewed clinical study, Swift Medical’s point-of-care visioning technology has demonstrated measurement accuracy and consistency exceeding the prevailing paper ruler method and other technologies.
The results showed Swift Skin and Wound produced 95%+ consistency between wound measurements. This means that if 5 different clinicians all took a measurement of the same wound with the application, they would all receive the same measurement every time – within 5%. The study also showed 95%+ accuracy in wound measurements with the application.
Swift Skin and Wound can help you transform your wound care practice by rooting your care decisions in consistent and reliable wound measurements. No longer will you need to worry about the inconsistency between clinicians or wonder if a wound is actually healing or not. With Swift Skin and Wound, you can empower all of your clinicians to practice at their peak, gain visibility into wound healing across your population and be confident in your staff and care plan.